Session Information
Date: Monday, November 11, 2019
Title: Systemic Sclerosis & Related Disorders – Basic Science Poster
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Pulmonary arterial hypertension (PAH) affects approximately 10% of patients with systemic sclerosis (SSc) and is a leading cause of death. Screening algorithms using clinical parameters have been developed to identify patients at high risk for PAH who should undergo confirmatory right heart catheterization (RHC). We sought to identify serum cytokines that might be useful in risk stratification of SSc patients for this potentially fatal complication.
Methods: Subjects were enrolled in the Pulmonary Hypertension Assessment and Recognition of Outcomes in Scleroderma (PHAROS), a multi-center prospective registry that includes SSc patients with 1) incident PAH based on RHC; 2) at high risk for PAH. High risk patients had a diffusion capacity for carbon monoxide (DLCO) < 55% predicted with a forced vital capacity (FVC) of >70% predicted, FVC/DLCO ratio >1.6, or right ventricular systolic pressure (RVSP) ≥40 mmHg on echocardiography. Low risk patients were enrolled at Stanford and had a DLCO ≥ 80%, FVC ≥ 80%, and RVSP ≤35mmHg or normal echocardiogram if no measurable tricuspid regurgitant jet was observed. Serum was available from 71 high risk patients, 81 incident PAH patients, 10 low risk patients, and 20 healthy controls (HC). A custom 14-plex array was used for cytokine analysis. Samples were normalized by background correction and removed if correlation between technical replicates was < 0.8. Cytokine expression was compared between patient groups by principal component analysis and Tukey’s test result. A multiple hypotheses corrected p-value < 0.05 was considered significant.
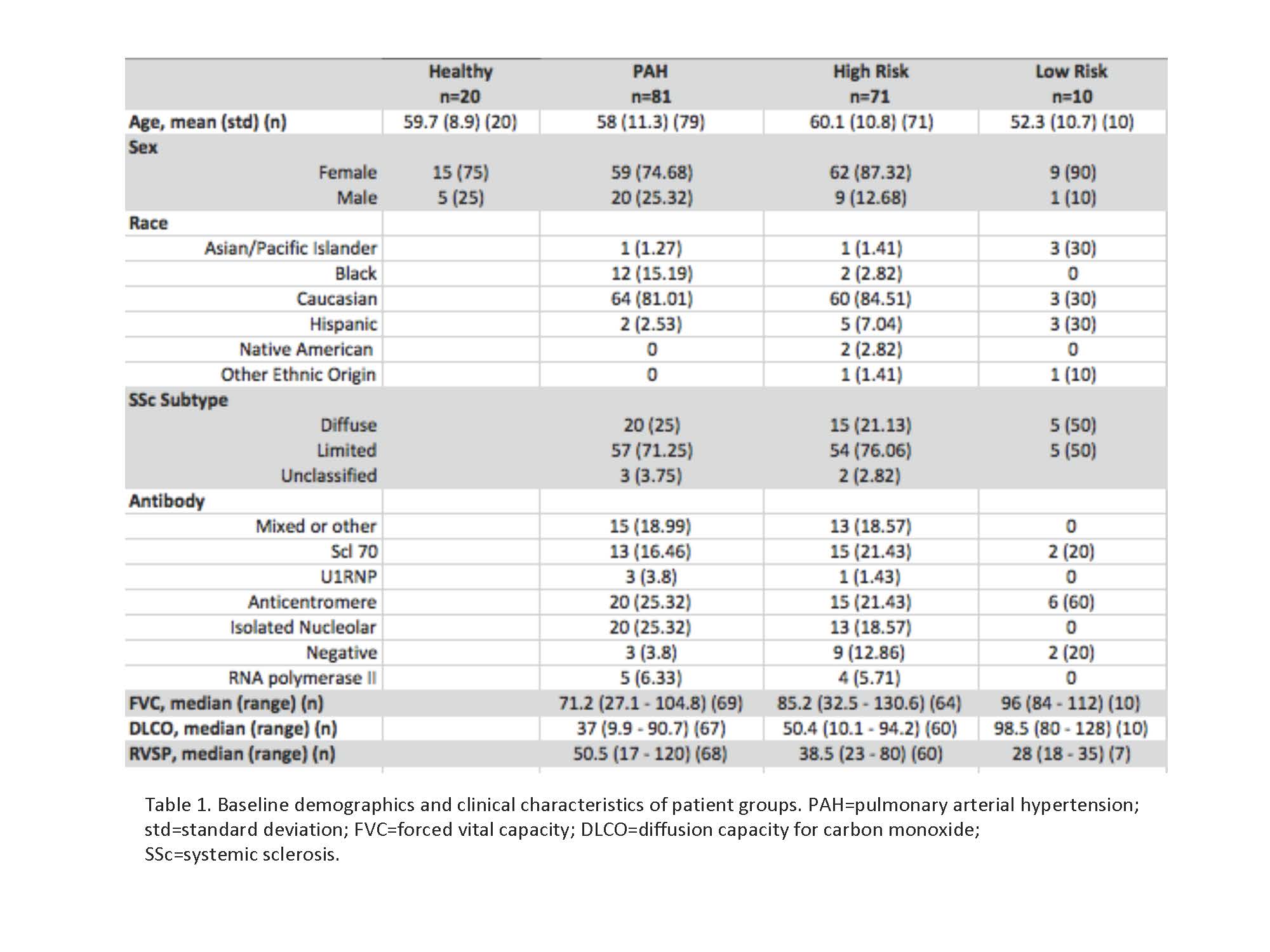
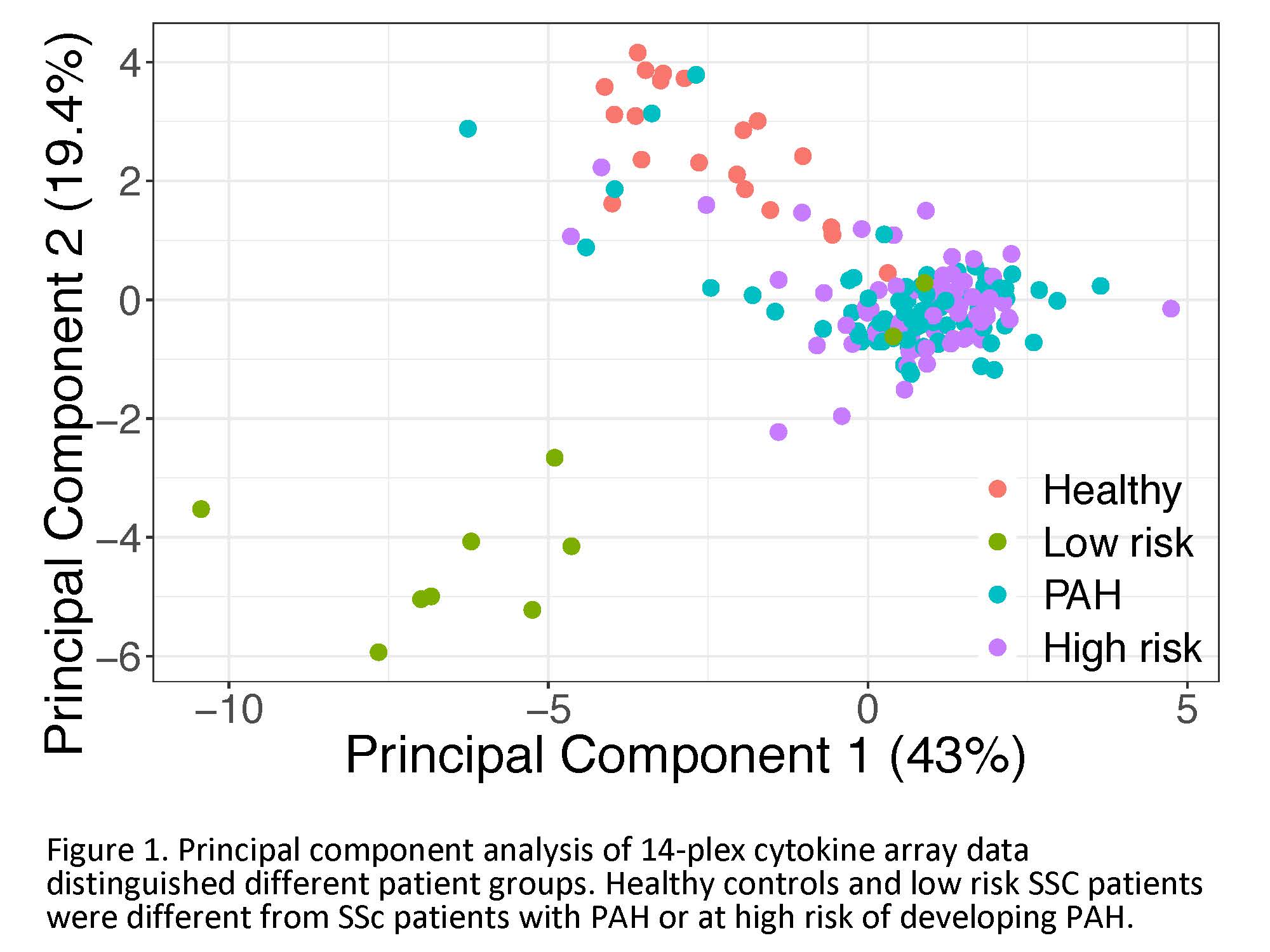
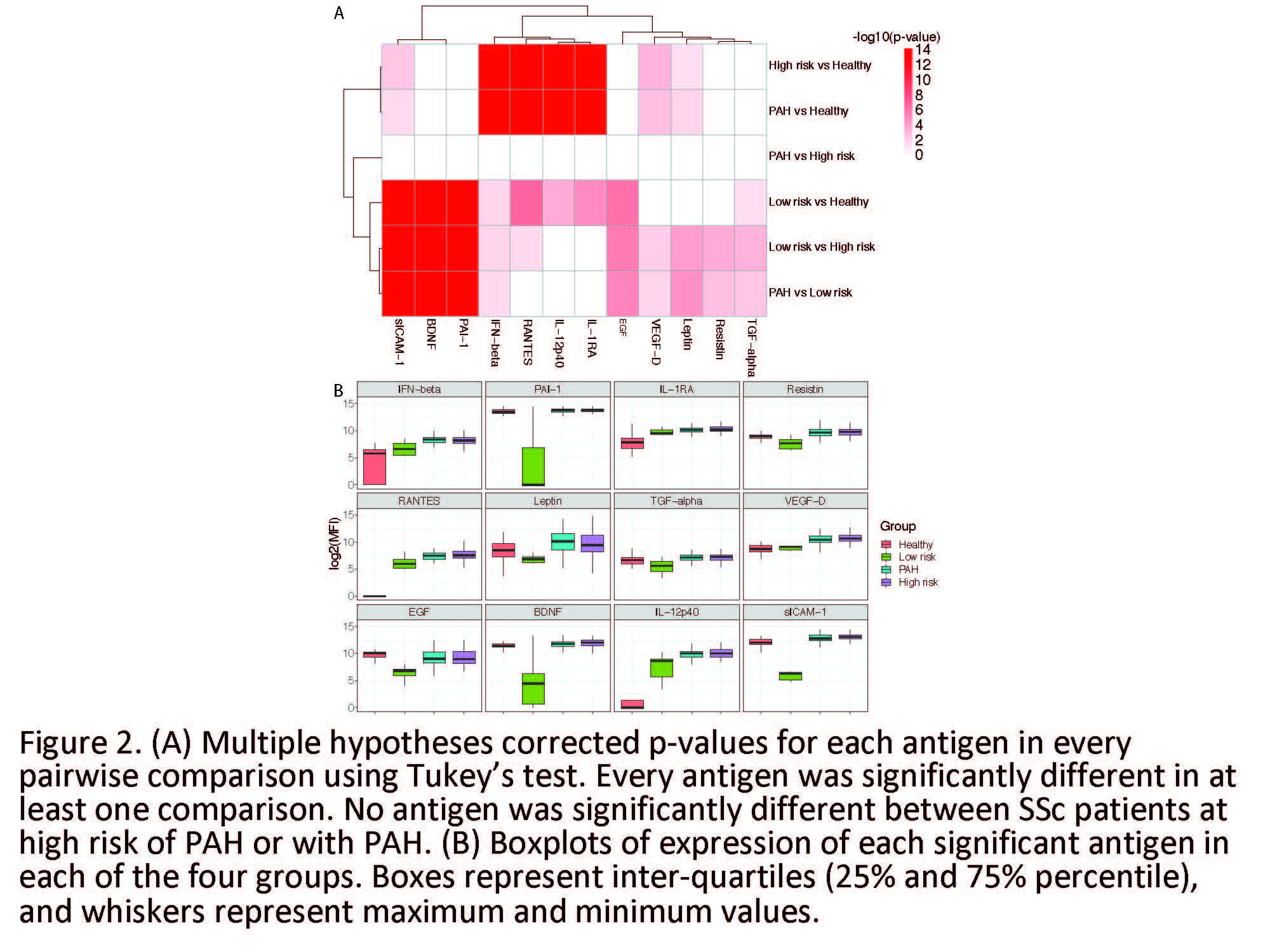
Results: Baseline characteristics of each patient group are described in Table 1. Two cytokines (sVCAM-1 and PDGF-BB) were removed from further analysis due to low correlation on replicate testing. Principle component analysis showed unique clustering for each patient group (Figure 1). We found that there was a significant difference in cytokine expression in at least one group comparison for every cytokine. Overall, there was very little difference in cytokine expression comparing high risk and PAH patient groups; however, these groups had substantially different cytokine profiles compared to low risk patients. In particular, low expression of PAI-1, EGF, BDNF, and sICAM-1 differentiated the low risk group from the high risk and PAH groups, as well as from HC. Higher levels of RANTES and IL-12p40 differentiated the three SSc groups from HC (Figure 2).
Conclusion: These data suggest that cytokine profiles can identify SSc patients who are at high risk for PAH. However, high risk and PAH patients had very similar cytokine profiles, suggesting that these patients are on a disease continuum. Our results need to be validated in an independent cohort of SSc patients.
To cite this abstract in AMA style:
Kolstad K, Khatri A, Donato M, Chang S, Li S, Steen V, Utz P, Khatri P, Chung L. Cytokine Signatures Differentiate Systemic Sclerosis Patients at High versus Low Risk for Pulmonary Arterial Hypertension [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/cytokine-signatures-differentiate-systemic-sclerosis-patients-at-high-versus-low-risk-for-pulmonary-arterial-hypertension/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cytokine-signatures-differentiate-systemic-sclerosis-patients-at-high-versus-low-risk-for-pulmonary-arterial-hypertension/