Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: COVID-19 in patients with rheumatoid arthritis (RA) is poorly understood. A recent study of mostly men with RA demonstrated increased COVID-19 risk in RA patients and more severe outcomes compared to matched non-RA patients; however, generalizability may be limited and findings need to be confirmed. We analyzed COVID-19 risk factors within RA patients overall and compared to those with osteoarthritis (OA) from our large musculoskeletal hospital during the initial wave of the pandemic in New York City.
Methods: We emailed a secure web-based survey to 26,045 patients ≥18 years old evaluated at least once by a rheumatologist between 2018-2020. Patients completed the survey between April 24, 2020-July 1, 2020. We collected data on demographics, COVID-19, medical history, and medication use. COVID-19 was suspected if the diagnosis was provided by a healthcare worker, and confirmed by a positive nasopharyngeal PCR antigen test. The former was included due to the lack of available testing early in the pandemic. ICD-10-CM algorithms were used to identify RA and OA. We used descriptive statistics as appropriate to compare patients with and without COVID-19 among RA and OA patients. We also compared RA versus OA subgroup of patients with COVID-19.
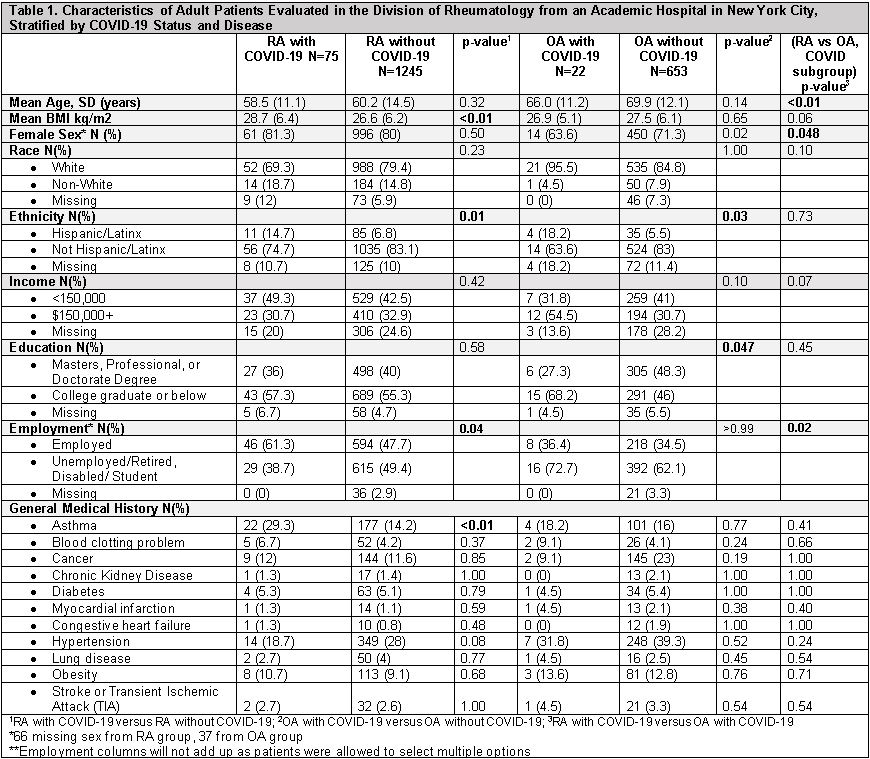
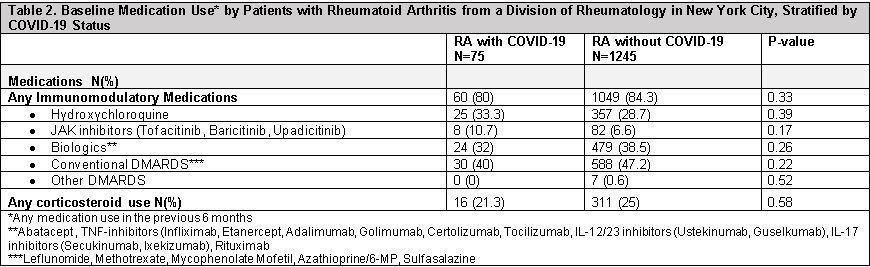
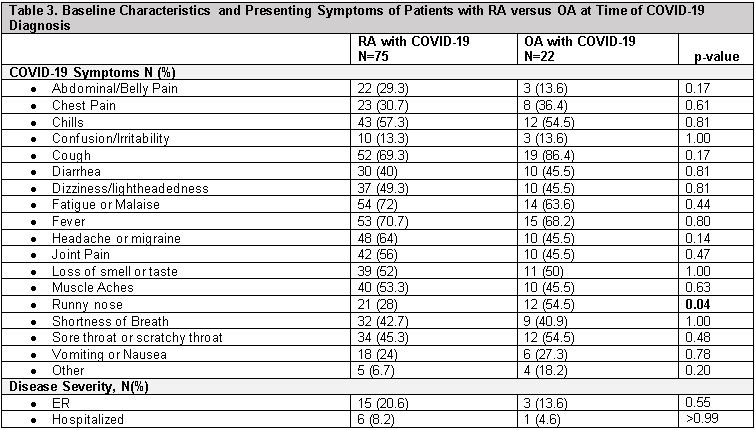
Results: Of the 6,583/26,045 (27.1%) patients who responded to our survey, 1,320 (20.1%) had RA and 675 (10.3%) had OA. Mean age of RA patients was 60.2 [14.4] years and 84.0% were female; mean age of OA patients was 69.7[12.1] years, and 75.2% were female. 5.7% of RA patients and 3.3% of OA patients self-reported COVID-19 (p=0.02). Compared to RA patients without COVID-19, RA patients with COVID-19 had higher BMI, were more likely to be Hispanic/Latinx and employed, and to have underlying asthma (Table 1). No difference in baseline steroid use or immunomodulatory medications were noted (Table 2). OA patients with COVID-19 were younger, more likely to be male and Hispanic/Latinx, and had higher education compared to OA without COVID-19; no differences in race, income, employment or general medical history were noted (Table 1). RA patients with COVID-19 were younger (58.5[11.1] vs. 66.0[11.2] years), more likely to be female (81.3% vs. 63.6%) and employed (61.3% vs. 36.4%) than OA with COVID-19; no differences in general medical problems were noted. Although RA patients with COVID-19 had a non-significantly higher prevalence of abdominal pain, headaches, joint pain, vomiting, and fatigue, OA patients had significantly higher rhinorrhea (Table 3). ER visits and hospitalization were similar in RA versus OA patients with COVID-19 (Table 3).
Conclusion: In a cohort of rheumatology outpatients in New York City during the early pandemic surge, COVID-19 incidence was higher in RA versus OA patients, but there was no difference in ER or hospitalization. In RA patients COVID-19 was associated with higher BMI, Hispanic/Latinx ethnicity, being employed, and a history of asthma. In OA patients, COVID-19 was associated with younger age, Hispanic race/ethnicity, and lower education. These findings are hypothesis generating and will be evaluated prospectively using multivariable analyses to help identify predictors of COVID-19 in potentially high risk patients.
To cite this abstract in AMA style:
Levine J, Bykerk V, Lally L, Mandl L, Barbhaiya M. COVID-19 in Patients with Rheumatoid Arthritis Compared to Patients with Osteoarthritis During the Pandemic in New York City [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/covid-19-in-patients-with-rheumatoid-arthritis-compared-to-patients-with-osteoarthritis-during-the-pandemic-in-new-york-city/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-in-patients-with-rheumatoid-arthritis-compared-to-patients-with-osteoarthritis-during-the-pandemic-in-new-york-city/