Session Information
Date: Monday, November 13, 2023
Title: (1013–1032) Healthcare Disparities in Rheumatology Poster II: Socioeconomic Determinants
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Medication nonadherence is a challenging issue in the management of systemic autoimmune rheumatic diseases (SARDs), leading to poor clinical outcomes. Although it is complex and multifaceted, cost is a significant barrier to medication adherence. We investigated cost-related medication burden in patients with SARDs, compared to that in patients without SARDs in a large diverse cohort across the U.S..
Methods: Among the participants with baseline survey and electronic health records in the All of Us (AoU) research program v7, we identified patients with SARDs who had ≥2 International Classification of Diseases (ICD)-9/10 and Systematized Nomenclature of Medicine (SNOMED) codes ≥ 60 days apart within two years.Cost-related medication burden was assessed in 3 ways using self-reported questionnaire data collected at enrollment: 1) unaffordability of prescription medicines, 2) cost-related medication nonadherence—skipping medications, taking less medicines, or delaying filling a prescription, and 3) cost-reducing strategies—asking for a lower cost medication, buying prescription drugs from another country, or using alternative therapies. Self-reported responses to each question were compared between patients with and without SARDs using Chi-squared tests. Logistic regression analyses calculated odds ratios (ORs), adjusting demographic, socioeconomic, and multiple clinical factors.
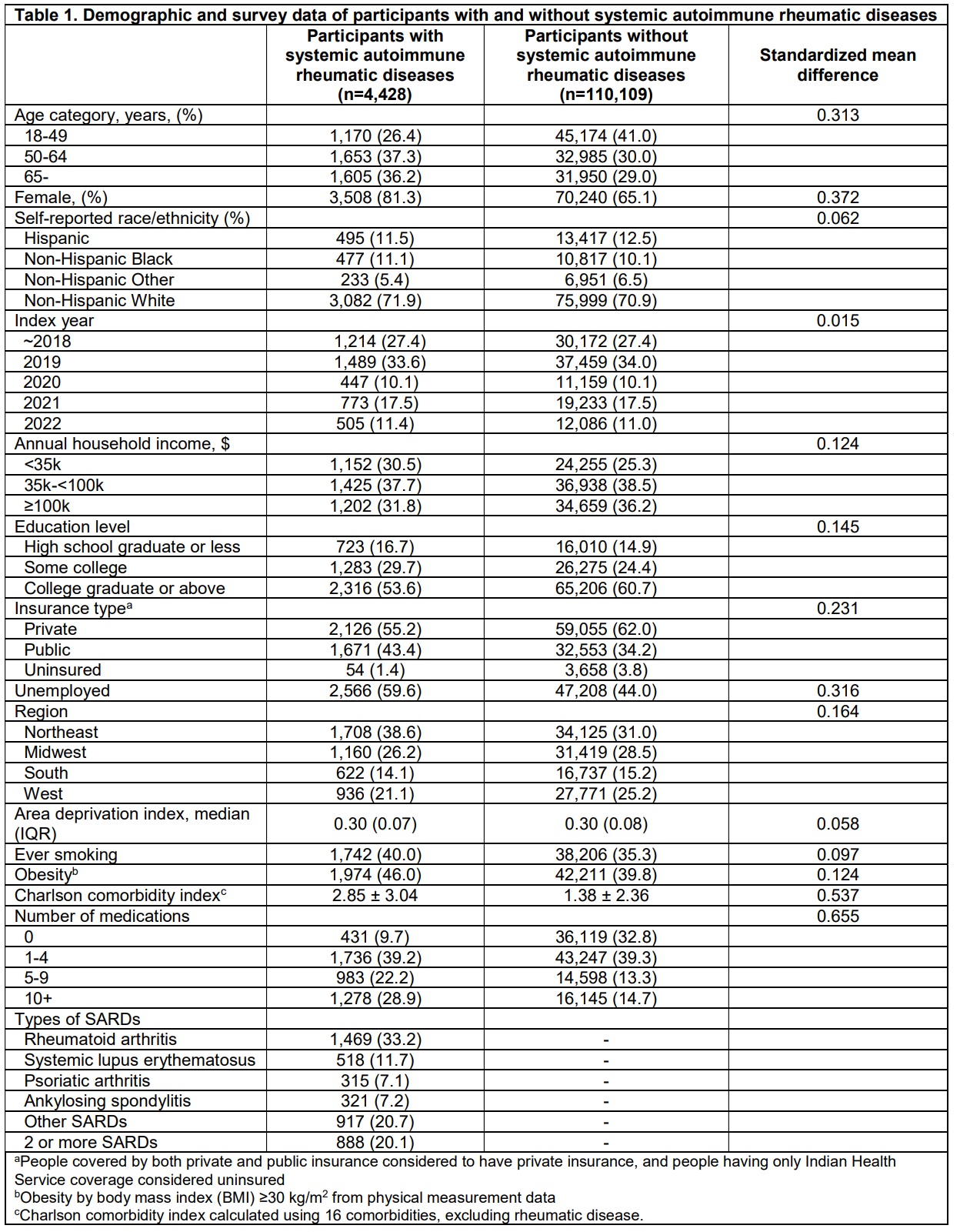
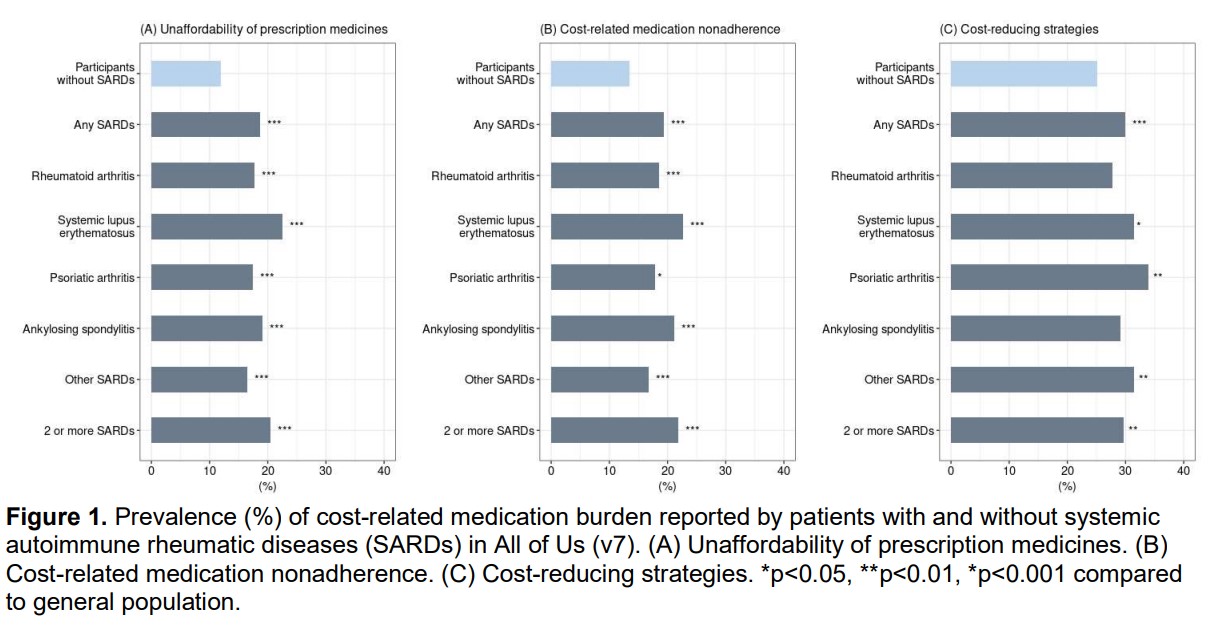
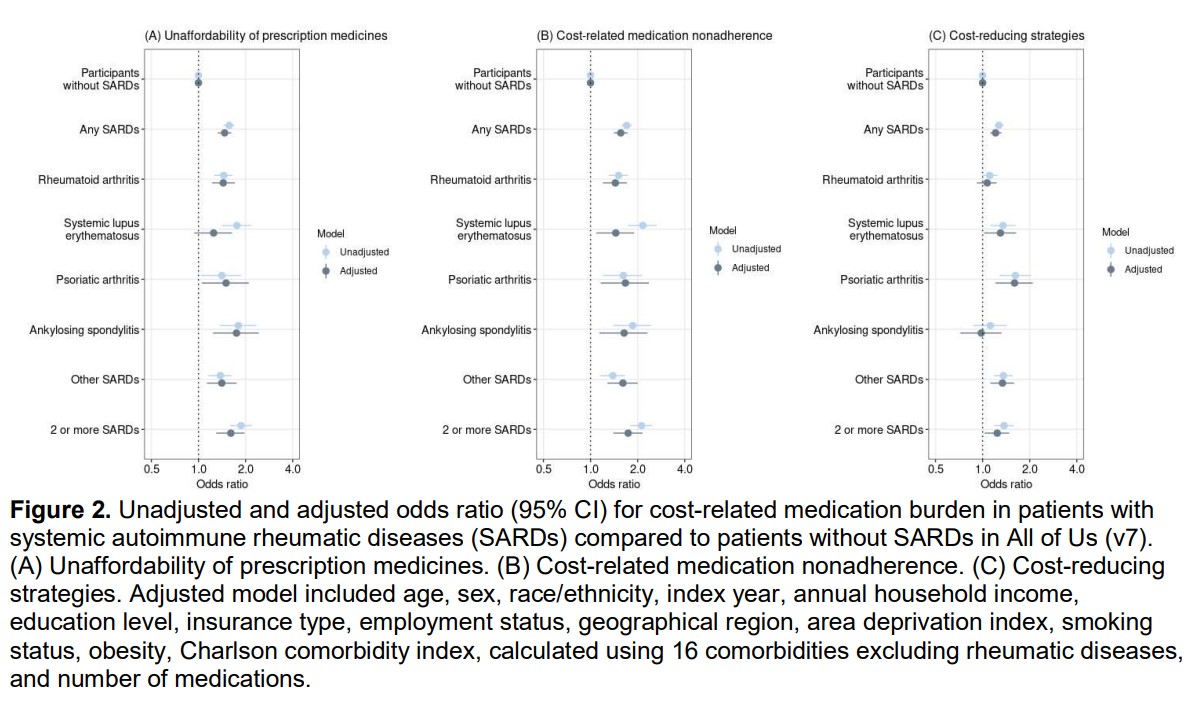
Results: Among respondents who fully answered these questionnaires, a total of 4,428 SARDs patients and 110,109 participants without SARDs were analyzed (Table 1). Patients with SARDs had lower socioeconomic status than those without SARDs. Among those with SARDs, 18.2% did not get prescription medicines due to cost, whereas this was 11.6% of those without SARDs (Figure 1). 18.7% of those with SARDs vs. 12.8% without SARDs reported cost-related medication nonadherence, while 29.9% with vs. 25.2% without SARDs reported using medication cost-reducing strategies. After adjusting for multiple demographic and clinical factors, patients with SARDs had 1.6-fold (95% CI 1.4-1.7) odds of reporting unaffordability of prescription medicines, 1.5-fold (95% CI 1.3-1.6) odds of reporting cost-related medication nonadherence, and 1.2-fold (95% CI 1.1-1.3) odds of reporting using cost-reducing strategies, than those without SARDs (Figure 2). Full adjustment reduced the odds of all 3 cost-reducing behaviors the most for those with SLE, likely as this is a younger, more diverse population of lower socioeconomic status than other SARDs groups.
Conclusion: Higher proportions of patients with SARDs self-reported unaffordability of prescription medicines, cost-related medication nonadherence, and cost-reducing strategies than did patients without SARDs in the large AoU research program, even after adjusting for multiple demographic and clinical factors. Ongoing research is investigating how cost-related medication burden influences adherence and clinical outcomes for patients with SARDs. Clinicians and other stakeholders should consider the financial burden of medications faced by patients with SARDs to improve medication adherence and thus clinical outcomes.
To cite this abstract in AMA style:
Yee J, Feldman C, Oakes E, Ellrodt J, Choi M, Karlson E, Costenbader K. Cost-related Medication Burden for Patients with and Without Systemic Autoimmune Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/cost-related-medication-burden-for-patients-with-and-without-systemic-autoimmune-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cost-related-medication-burden-for-patients-with-and-without-systemic-autoimmune-rheumatic-diseases/