Session Information
Session Type: Combined Abstract Sessions
Background/Purpose: Community based outpatient clinics (CBOCs) have been established by the Department of Veteran Affairs (VA) to provide primary care services to veterans living in remote and rural regions. While CBOCs provide excellent primary care services, the current model does not allow providers in CBOCs to develop and deliver specialty services. The objective of this study was to evaluate the cost-effectiveness of training rural primary care providers to perform knee injections in CBOCs, rather than referring the patient to an urban medical center with rheumatology and orthopaedic specialists. Referral often involves significant travel for patients in rural areas.
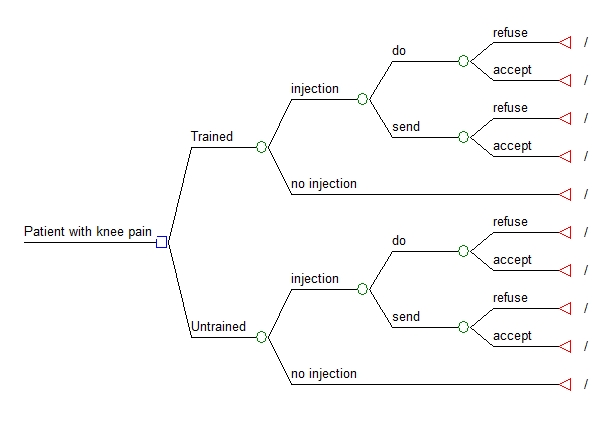
Methods: We developed a decision analytic model to compare costs and outcomes between rural providers who are trained to perform knee injections and those who are not trained. In the model, each type of provider is presented with a hypothetical patient who has knee pain and should receive an injection. Costs included in the model (including medical management for patients who do not receive an injection, training of the rural provider to perform injections, travel reimbursement for patients who are sent to an urban medical center) were from the perspective of the VHA. The effectiveness outcome was quality-adjusted life years (QALYs). In our primary analysis, a range of values were used for 2 key inputs: the number of patients with knee pain presenting to the rural clinic in 1 year period (range:10-100) and the average distance from the patients’ home address to the urban medical center (range:50-500). Probabilistic sensitivity analyses were performed using 1,000 2nd order Monte Carlo simulations and the benefits of knee injection were assumed to last 90 days.
Results: In our base case analyses (which assumed 30 patients per year presenting with knee pain that could benefit from an injection and an average distance of 100 miles from the patient’s home adders to the urban medical center), the incremental cost-effectiveness ratio (ICER) for trained rural providers was $27,692/QALY. ICERs were more sensitive to the number of patients than to distance Table 1. Training rural providers was cost-effective in 68.6% of 1,000 Monte Carlo simulations at a willingness to pay threshold of $50,000/QALY.
|
Incremental cost effectiveness ratios for range of values for average distance and number of patients per year (US dollars/QALY) |
||||
|
|
Number of patients |
|||
|
Distance |
10 |
30 |
50 |
100 |
|
50 |
$70,732 |
$27,888 |
$19,319 |
$12,893 |
|
100 |
$70,536 |
$27,692 |
$19,124 |
$12,697 |
|
200 |
$70,145 |
$27,301 |
$18,732 |
$12,305 |
|
500 |
$68,970 |
$26,126 |
$17,557 |
$11,130 |
Conclusion: Training rural providers to perform knee injections for patients with knee pain appears cost-effective at the commonly used threshold of $50,000/QALY if sufficient numbers of such patients are seen at rural primary care clinics. We are currently implementing such a training program to test the validity of these projections.
Disclosure:
M. J. Battistone,
None;
R. E. Nelson,
None;
W. D. Ashworth,
None;
A. Barker,
None;
M. Grotzke,
None;
T. A. Huhtala,
None;
R. Z. Tashjian,
None;
G. W. Cannon,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cost-effectiveness-of-training-rural-providers-to-perform-joint-injections/