Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a complex autoimmune disease with diverse manifestations, including thrombotic thrombocytopenic purpura (TTP), a life-threatening hematologic disorder. The pathogenesis of acquired TTP (aTTP) in SLE is believed to involve formation of autoantibodies against ADAMTS13, which inhibit this matrix metalloproteinase activity, thus inhibiting the cleavage of von Willebrand factor multimers and ultimately promoting platelet aggregation and leading to microvascular thrombosis. The clinical overlap between SLE flares and aTTP poses significant diagnostic and therapeutic challenges. This study aims to assess the prevalence, clinical characteristics, and management of aTTP in SLE patients.
Methods: We conducted a retrospective cohort study using the Cosmos Cohort, an integrated database with nearly 296 million patient encounters from multiple US healthcare systems. We searched all encounters from March 31, 2015 to March 5, 2025 for aTTP cases using the grouper name “thrombotic microangiopathy” and included all subsets. We then identified SLE patients using the grouper name “systemic lupus erythematosus” and included all subsets. We then combined both datasets to analyze population characteristics. To compare with local data, we extracted SLE and aTTP cases from our institutional dataset using Epic SlicerDicer and performed a comparative analysis of prevalence, demographics, and treatment patterns.
Results: Among 751,633 SLE patients in the Cosmos Cohort, 1,610 (0.21%) were diagnosed with aTTP, with a female predominance (1,346 females, 264 males; 83.6% female). In our institutional dataset of 1,397 SLE patients, the prevalence was slightly higher at 0.29% (4 patients: 2 females, 2 males). The mean age was 46 years in the Cosmos Cohort and 60 years in our dataset. SLE activity showed Kidney involvement in 60.6% (976 patients, lung involvement in 9% (143 patients), pericarditis in 7.9% (127 cases) and other organ or system involvement in 41% (653 patients). There was a history of renal biopsy in 525 patients. Treatments in the Cosmos Cohort included rituximab (28.6%, 460 patients), mycophenolate mofetil (47.5%, 764 patients), and cyclophosphamide (14%, 225 patients).12 patients received plasma exchange (PLEX) therapy. In our dataset, 3 of 4 patients (75%) received rituximab, while the treatment for the remaining patient was unknown. A total of 397 patients in the Cosmos cohort are currently deceased, however the cause of death and relationship to aTTP and SLE are unknown.
Conclusion: SLE-associated aTTP is a rare yet severe complication requiring early detection and aggressive treatment. Our study describes its prevalence in the modern era of immunosuppression, highlights differences in prevalence and treatment approaches across datasets, and emphasizes the need for standardized guidelines. Further research, including multi-center prospective studies, would be beneficial to establish a more comprehensive understanding of aTTP prevalence in SLE patients across different populations and settings and investigate effectiveness of treatment approaches.
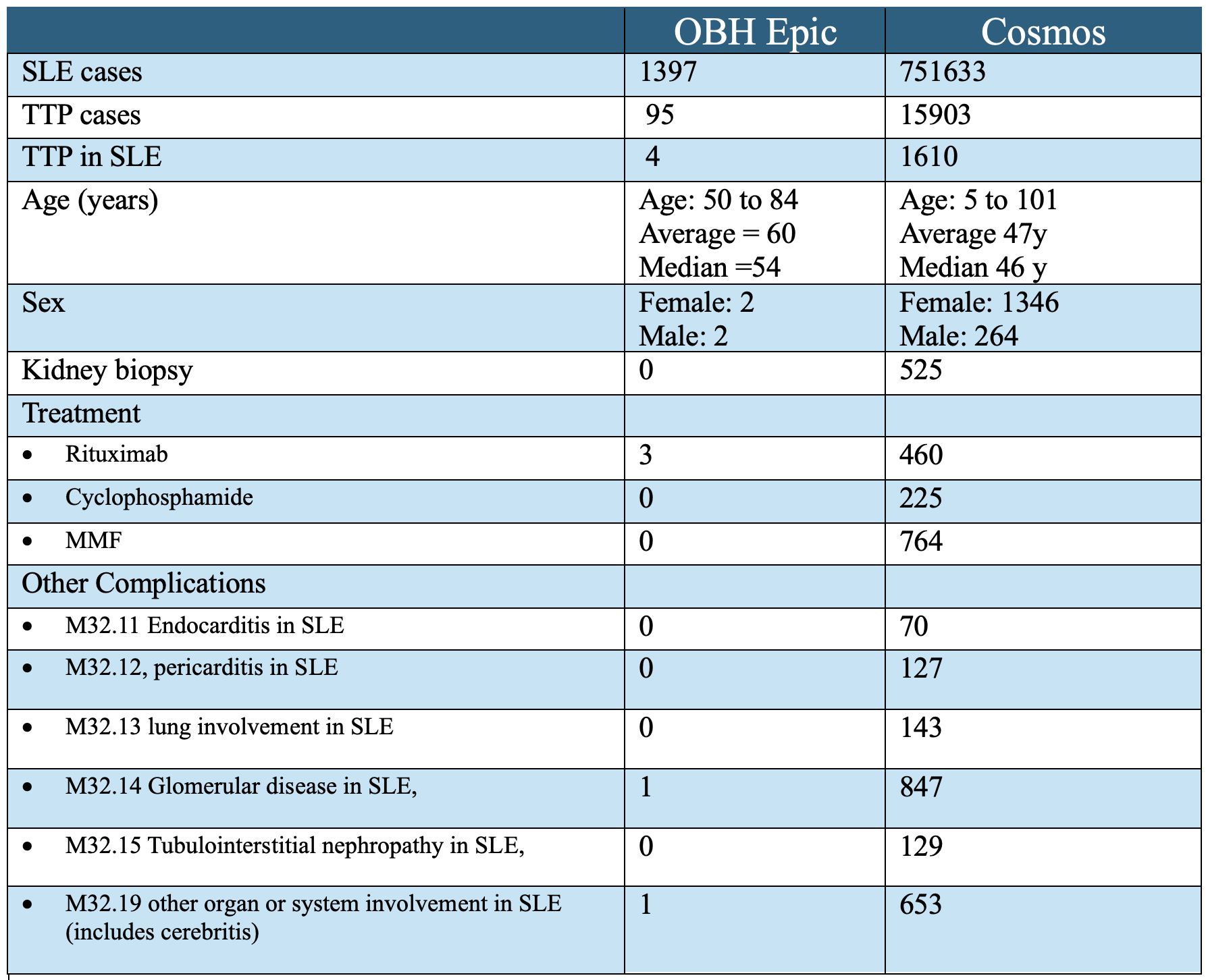 Table 1 compares number of SLE and aTTP cases from COSMOS and our institutional dataset by age, sex, treatment, and complications.
Table 1 compares number of SLE and aTTP cases from COSMOS and our institutional dataset by age, sex, treatment, and complications.
To cite this abstract in AMA style:
Sapkota N, Andriushchenko Y, Malik S, Choi S, Terebelo S. COSMOS Prevalence of aTTP in SLE [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/cosmos-prevalence-of-attp-in-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cosmos-prevalence-of-attp-in-sle/
