Session Information
Date: Saturday, November 12, 2022
Title: Abstracts: SLE – Diagnosis, Manifestations, and Outcomes I: Renal Aspects
Session Type: Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Lupus nephritis is a leading cause of morbidity in patients with systemic lupus erythematosus (SLE). We sought to determine the incidence of lupus nephritis (LN) in a contemporary United States SLE cohort.
Methods: We used observational data from TriNetX, an electronic health record (EHR) database from 46 health care organizations across the United States, including academic medical centers, community hospitals, and outpatient facilities, to identify an inception cohort of patients with SLE. We identified all patients who were enrolled for at least 5 years prior to the first ICD 9/10 code for SLE and then met the definition of SLE (≥2 ICD codes ≥30 days and ≤2 years apart) between January, 2005 and August, 2021. We identified patients who developed LN, defined as ≥1 ICD-10 code for LN or ≥2 clinical indicators of nephritis, including ICD-9 580-586, 791.0; ICD-10 N00, N04, N05, N17, N18, R80.9 (Chibnik 2010). Patients meeting this definition within 6-months after the first SLE code were considered to have early LN. We also assessed a secondary LN definition, requiring ≥1 ICD-10 code for LN or ≥2 clinical indicators of nephritis + a kidney biopsy or new LN treatment (i.e., glucocorticoids, azathioprine, mycophenolate, cyclophosphamide, rituximab, tacrolimus, or cyclosporine) within 6-months of the nephritis codes. We assessed demographics, comorbidities, medications, disease severity (SLE severity Index, Garrison 2013), geographic location, and healthcare utilization at the index date of entering the SLE inception cohort, and we compared these factors between patients with and without LN at SLE onset. Patients were followed until the diagnosis of LN, death, disenrollment from the database, or end of the study period. We assessed the cumulative incidence of LN among patients with SLE, stratified by sex and race/ethnicity, accounting for the competing risk of death.
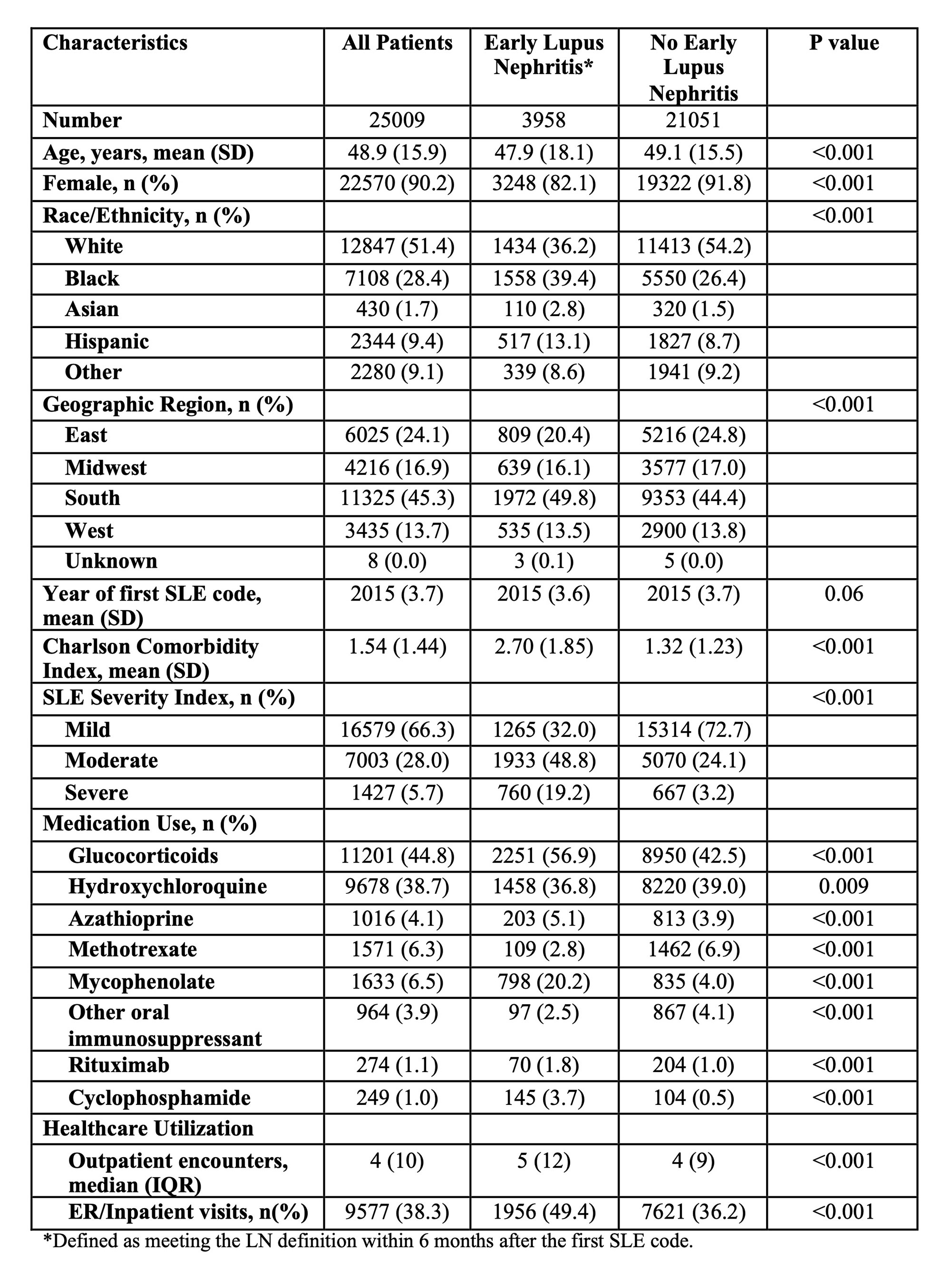
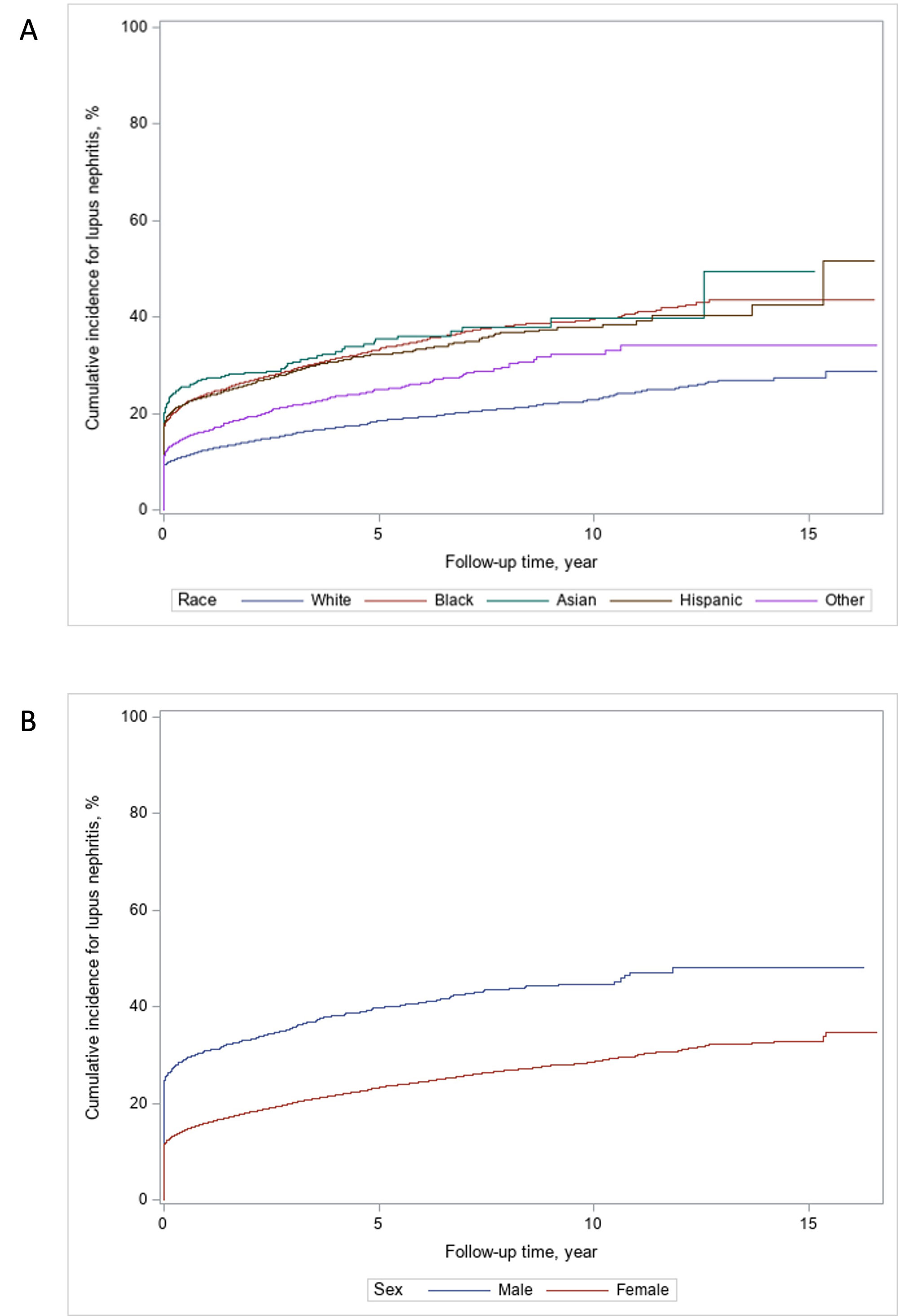
Results: We identified 25,009 patients in the SLE inception cohort. 3,958 (15.8%) had early LN; they were more likely to be black (39.4% vs 26.4%) or Hispanic (13.1% vs 8.7%) than those without early LN (Table 1). Those with early LN were younger on average, and a higher proportion were male and lived in the south. A total of 6,025 patients developed lupus nephritis during a mean of 50.2 months (SD 40.3) follow up, and 4,175 (69.3%) met the stricter secondary definition. The overall cumulative incidence of LN was 24.9% at 5 years, 30.1% at 10 years, and 34.4% at 15 years of follow up (Figure 1). The cumulative incidence was similar among black, Hispanic, and Asian patients (39.5%, 37.8%, and 39.9% at 10 years, respectively) and comparatively lower among white patients (22.9% at 10 years) (Figure 2). The incidence of LN was higher among men with SLE (44.7% vs 28.6% of women at 10 years).
Conclusion: In this contemporary, multi-center, EHR-based SLE inception cohort, one third of patients with SLE developed LN after 15 years of follow-up, and just over half of all cases were identified as an early manifestation around the time of SLE diagnosis. The incidence of LN was higher in non-white individuals and in men with SLE. Despite improved treatment for SLE in recent years, LN remains a frequent manifestation among patients with SLE that benefits from early identification and treatment.
To cite this abstract in AMA style:
Jorge A, Zhou B, Nestor J, zhang y, Choi H. Contemporary Incidence of Lupus Nephritis Among Patients with Systemic Lupus Erythematosus in the United States [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/contemporary-incidence-of-lupus-nephritis-among-patients-with-systemic-lupus-erythematosus-in-the-united-states/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/contemporary-incidence-of-lupus-nephritis-among-patients-with-systemic-lupus-erythematosus-in-the-united-states/