Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Connective tissue diseases (CTDs) are a category of autoimmune disease in which interstitial lung disease (ILD) is a common pulmonary manifestation. Due to the vast variety of CTDs, ILD patterns, and levels of severity, there are no clear guidelines for evaluating, monitoring, and treating in the multidisciplinary setting. This study aims to identify trends for CTD-ILD in our cohort, including diagnoses, prevalence, and treatments which may in the future aid in improving overall mortality and morbidity in patients.
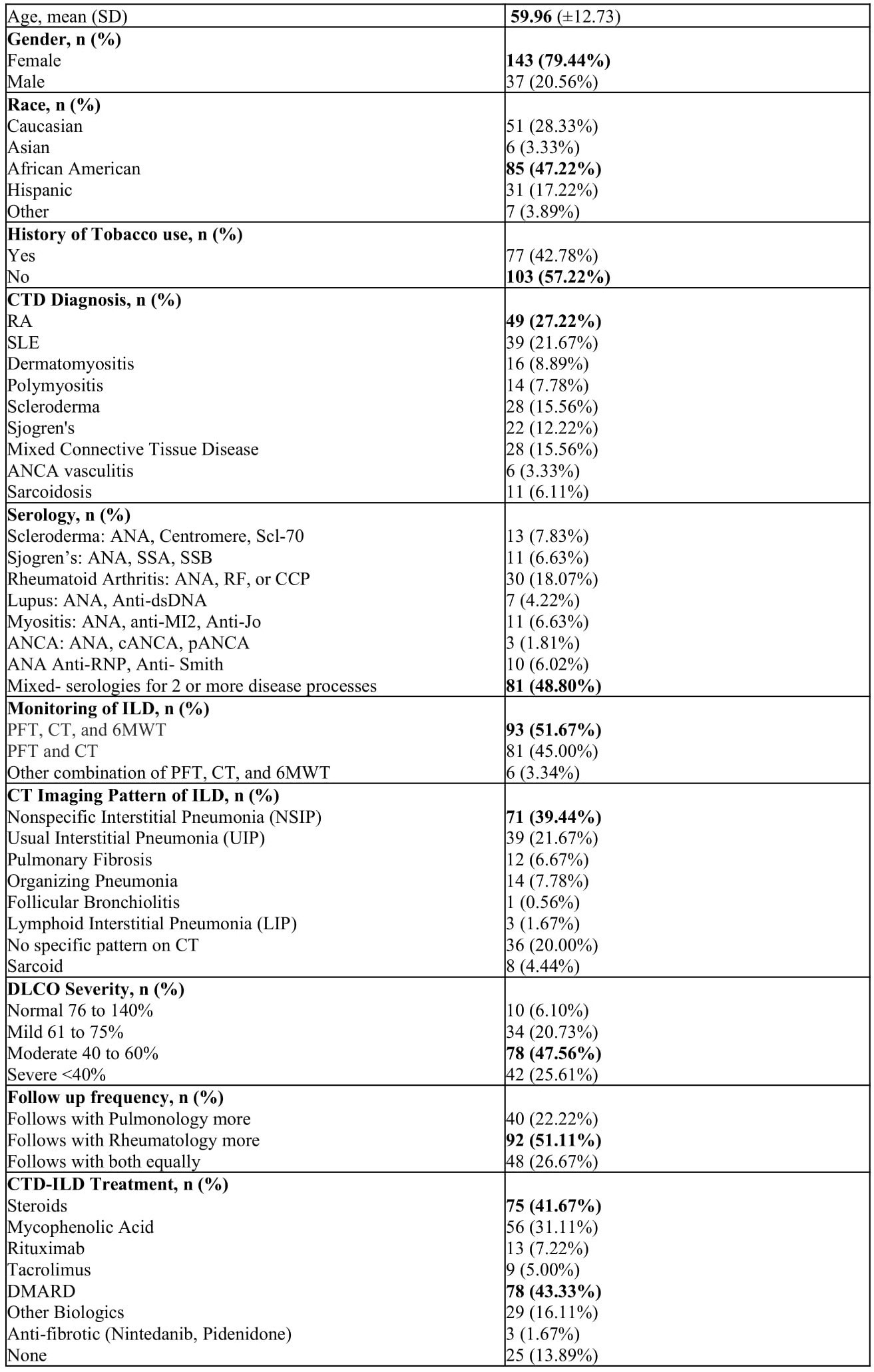
Methods: A single center retrospective study was performed on patients with ICD-10 diagnoses of CTDs (listed in Table 1) and ILD. Demographics, tobacco use, CTD diagnosis, serologies, monitoring tests for ILD such as computed tomography (CT), pulmonary function tests (PFTs), 6-minute walk tests (6MWTs), and diffusing capacity for carbon monoxide (DLCO) severity, frequency of rheumatology versus pulmonology follow-up, and treatments were recorded. Descriptive statistics were obtained. Pearson’s Chi-squared test, Fisher’s exact test, and one-way ANOVA were performed. A p value of ≤ 0.05 was considered significant.
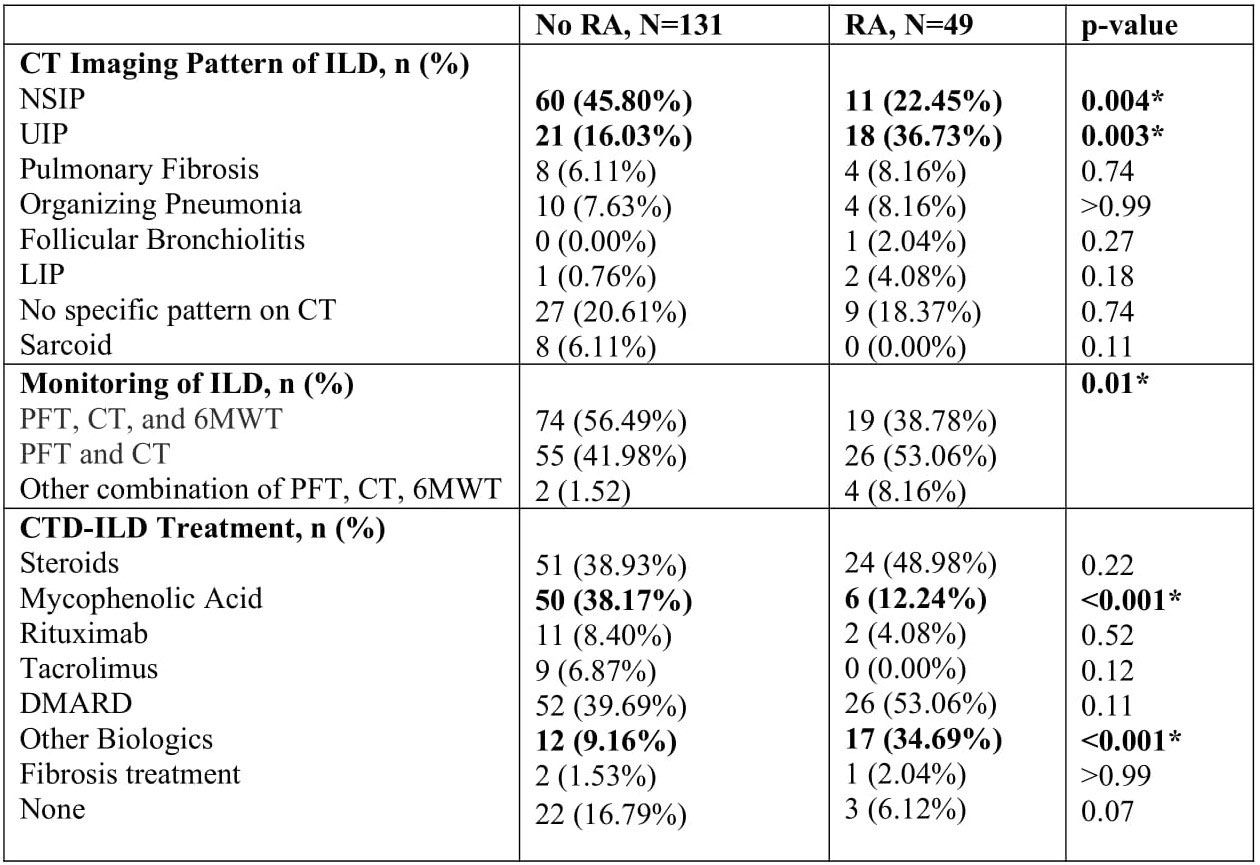
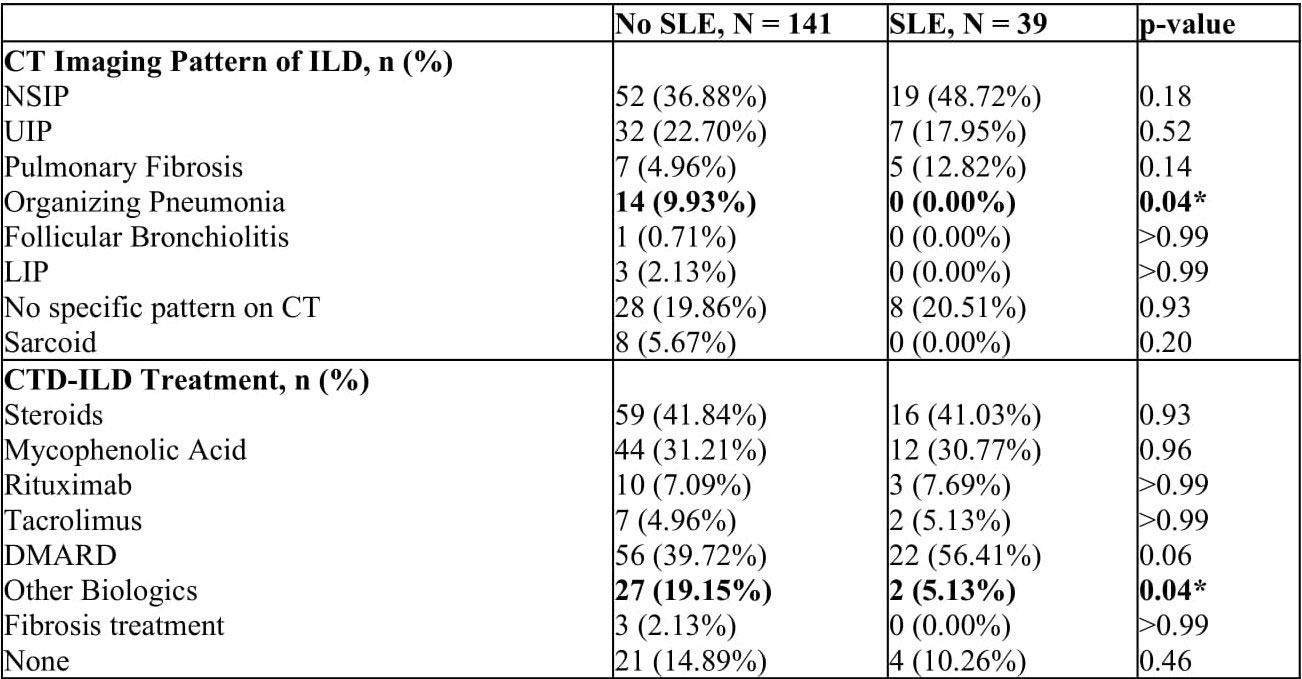
Results: Of 600 charts reviewed, 180 met inclusion criteria. Descriptive statistics in Table 1. The mean age was 60 with 79% being female. The most common ethnicity was African American. The most common CTD diagnosis was RA. 52% of patients were monitored with a combination of PFTs, CTs, and 6MWTs. Nonspecific interstitial pneumonia (NSIP) was the most common CT pattern. 48% had moderate DLCO severity. 89% followed rheumatology and pulmonology outpatient, but 51% followed rheumatology more frequently. The majority of patients were treated with steroids (42%) and DMARDs (43%). When comparing DLCO severity by ethnicity, Caucasians were more likely to have normal to mild lung disease as compared to African American patients who had more severe disease (p=0.01). Further analysis on the cohort’s two most common CTDs, RA and SLE, are summarized in Tables 2 and 3. For CT patterns: a higher percent of non-RA had NSIP (p=0.004) while a higher percent of RA had usual interstitial pneumonia (UIP) (p=0.003); a higher percent of non-SLE had organizing pneumonia (p=0.04). For treatments: a higher percent of non-RA used mycophenolic acid (p< 0.001) while a higher percent of RA used other biologics (p< 0.001); a higher percent of non-SLE patients used other biologics (p=0.04).
Conclusion: Like previous descriptive cohort studies on CTD-ILD, this study continues to identify significant trends. In this cohort, patients were predominantly female and African American. Regardless of disease or serologies, African Americans had the worse DLCO severity. Despite the development of new biologic therapies, many patients continue to be maintained on standard immunosuppressive treatment with steroids and DMARDs, whereas only the RA and non-SLE trended towards biologic use. Finally, despite the prevalence of ILD, rheumatology visits were more frequent than pulmonary visits alone. This underscores the importance of rheumatologists to screen and monitor for ILD symptoms in the management of all CTDs. These trends can help guide the care of patients in similar populations and guide more future prospective studies.
To cite this abstract in AMA style:
Sabharwal A, Liu Y, Rustomji Y, Khandelwal S. Connective Tissue Disease-Related Interstitial Lung Disease: Trends from an Urban Academic Tertiary Care Center [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/connective-tissue-disease-related-interstitial-lung-disease-trends-from-an-urban-academic-tertiary-care-center/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/connective-tissue-disease-related-interstitial-lung-disease-trends-from-an-urban-academic-tertiary-care-center/