Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial Lung Disease (ILD) in systemic sclerosis (SSc) is a common complication that has varied progression rate and prognosis. Different progression definitions include minimal clinically important worsening of forced vital capacity (FVC MCIW), EUropean Scleroderma Trials and Research group (EUSTAR) progression, Outcome Measures in Rheumatology Clinical Trials (OMERACT) progression, and INBUILD/ Erice ILD working group progression. The aim of the study was to assess the concordance and prognostic value of these different definitions in SSc-ILD patients overall and specific clinical subsets.
Methods: Progression status in consecutive SSc-ILD patients was assessed over 24 months, comparing SSc-ILD-related mortality between progressors and non-progressors according to different definitions over the following 60 months. The prediction performances of different progression definitions were investigated with Cox Regression analysis and compared using Akaike information criterion (AIC) with a difference greater than 2 considered as evidence in favor of the model with the smaller AIC.
Results: The 245 SSc-ILD patients enrolled had a mean age of 54.6± 3.2 years and a median disease duration of 4 (IQR 2-8) years from the first non-Raynaud symptoms. Among these patients, 18.8% were males, and 54.7% had the diffuse LeRoy cutaneous variant, 59.2% had anti-Scl70 positivity, and 14.3% anti-centromere antibody positivity.
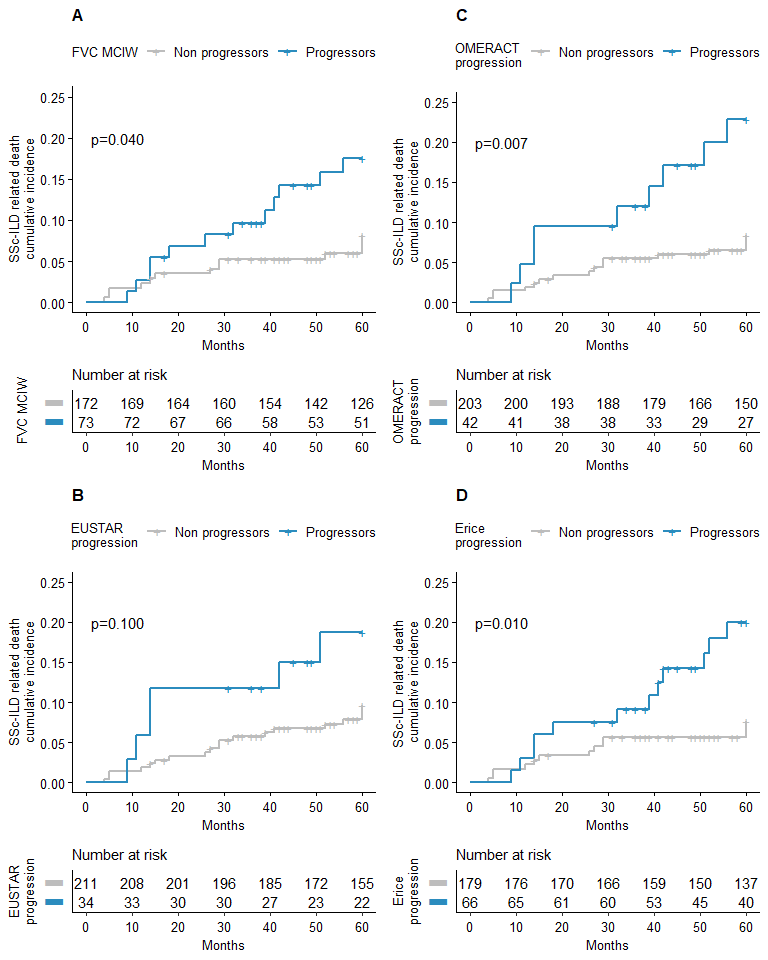
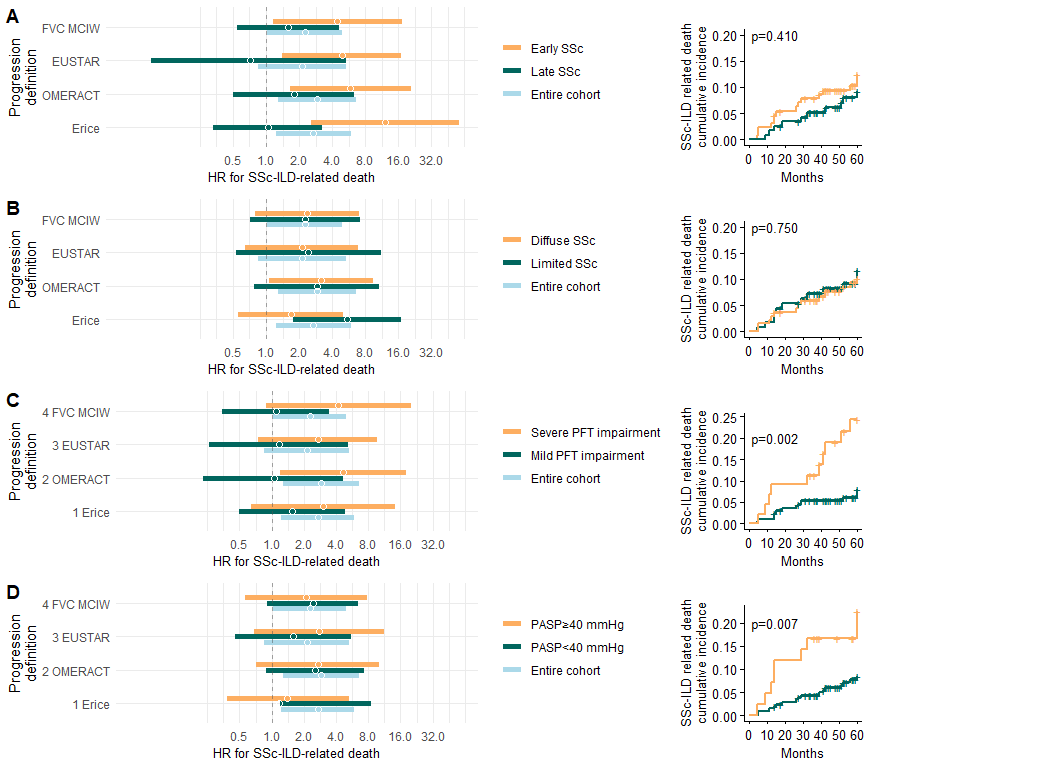
Twenty-six deaths were reported, and mortality was linked to progression per FVC MCIW (HR 2.27, 95% CI 1.03 – 4.97, p=0.041), OMERACT (HR 2.90, 95% CI 1.28 – 6.57, p=0.011), and INBUILD/Erice trial definitions (HR 11.02, 95% CI 2.38 – 51.08, p=0.002). Prognostic prediction using these four definitions was challenging in patients with longer disease duration, mild pulmonary function impairment, and pulmonary artery systolic pressure (PASP)≥40 mmHg. Erice criteria were superior in patients with disease duration >3 years, limited cutaneous variant, and PASP< 40 mmHg (ΔAIC >2). OMERACT criteria performed better in diffuse cutaneous variant patients with severe baseline functional impairment (ΔAIC >2).
Conclusion: The proposed SSc-ILD progression definitions are not interchangeable, risking potential misdiagnosis in up to a third of progressors. Regardless of criteria, progressors frequently showed diffuse skin disease variant, shorter disease duration, and worse functional impairment.
Four main definitions are compared: A) FVC MCIW, B) OMERACT definition, C) EUSTAR definition D) Erice definition. Abbreviations: EUSTAR EUropean Scleroderma Trials and Research group; FVC MCIW minimal clinical important worsening of forced vital capacity, OMERACT Outcome Measures in Rheumatology Clinical Trials, SSc-ILD scleroderma-related interstitial lung disease.
The patients were divided according to A) disease duration, B) LeRoy cutaneous variant, C) severity of baseline functional lung impairment and D) PASP values on echocardiography. The average risks of the whole population are also reported as comparators. The corresponding survival curves of the considered subgroup are displayed and compared on the right. Abbreviations: EUSTAR EUropean Scleroderma Trials and Research group; FVC MCIW minimal clinical important worsening of forced vital capacity, HR hazard ratio, OMERACT Outcome Measures in Rheumatology Clinical Trials, PASP pulmonary artery systolic pressure, PFT pulmonary function test, SSc-ILD scleroderma-related interstitial lung disease.
To cite this abstract in AMA style:
De Lorenzis e, Del Galdo F, Natalello g, Di Donato S, verardi l, Kakkar V, Cerasuolo p, Varone F, Richeldi L, D'Agostino M, Bosello S. Concordance and Prognostic Relevance of Different Definitions of Systemic Sclerosis Interstitial Lung Disease Progression [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/concordance-and-prognostic-relevance-of-different-definitions-of-systemic-sclerosis-interstitial-lung-disease-progression/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/concordance-and-prognostic-relevance-of-different-definitions-of-systemic-sclerosis-interstitial-lung-disease-progression/