Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Evaluation of Interstitial Lung Disease (ILD) progression relies on high resolution computed tomography (HRCT) and pulmonary function test (PFT). As we previously reported in our Idiopathic Inflammatory Myopathies (IIM) cohort, PFT and HRCT had poor agreement sometimes limiting ability to detect meaningful change. Computer Aided Lung Informatics for Pathology Evaluation and Rating (CALIPER) is a digital analysis of HRCT to provide objective measurement of parenchymal and vascular changes. To date, CALIPER has not been applied to HRCT in IIM-ILD.
Methods: This is a retrospective analysis of the Northwell Myositis cohort, meeting 2017 EULAR/ACR classification criteria for IIM with ILD, validated by HRCT. Patients with >2 PFTs and >2 HRCT chests were included. HRCTs were uploaded on the Imbio CALIPER platform which measured percentage of ground glass opacities (GGO), reticular pattern (RP), honeycombing, and pulmonary vascular volume (PVV) in total and 6 lung fields separately. Post- transplant imaging and PFTs on one patient were excluded from analysis. HRCT and PFT performed within 6 months were paired for correlation analysis. Absolute and annualized change of GGO, RP, PVV and FVC, DLCO were calculated. Traditional HRCT chest was recorded as improved, stable and worse as read by radiologist. Descriptive statistics, Kruskal Wallis test, Kappa statistics and Pearson correlation coefficient analysis were used to compare groups for continuous and categorical variables, respectively.
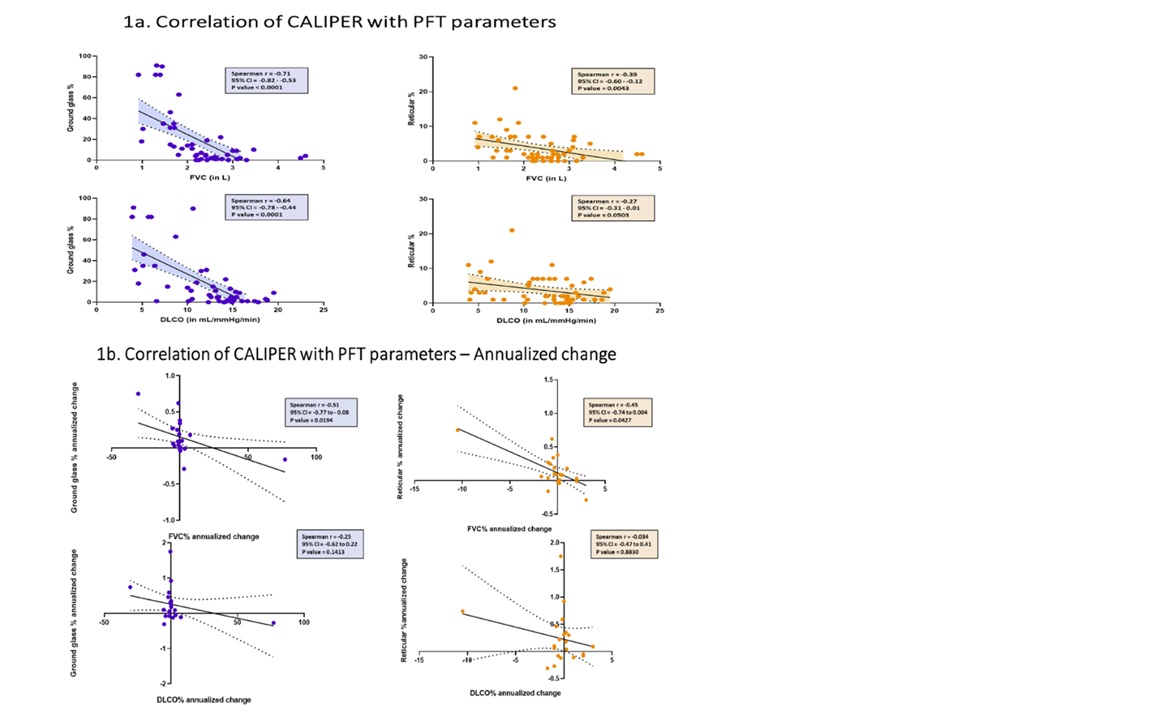
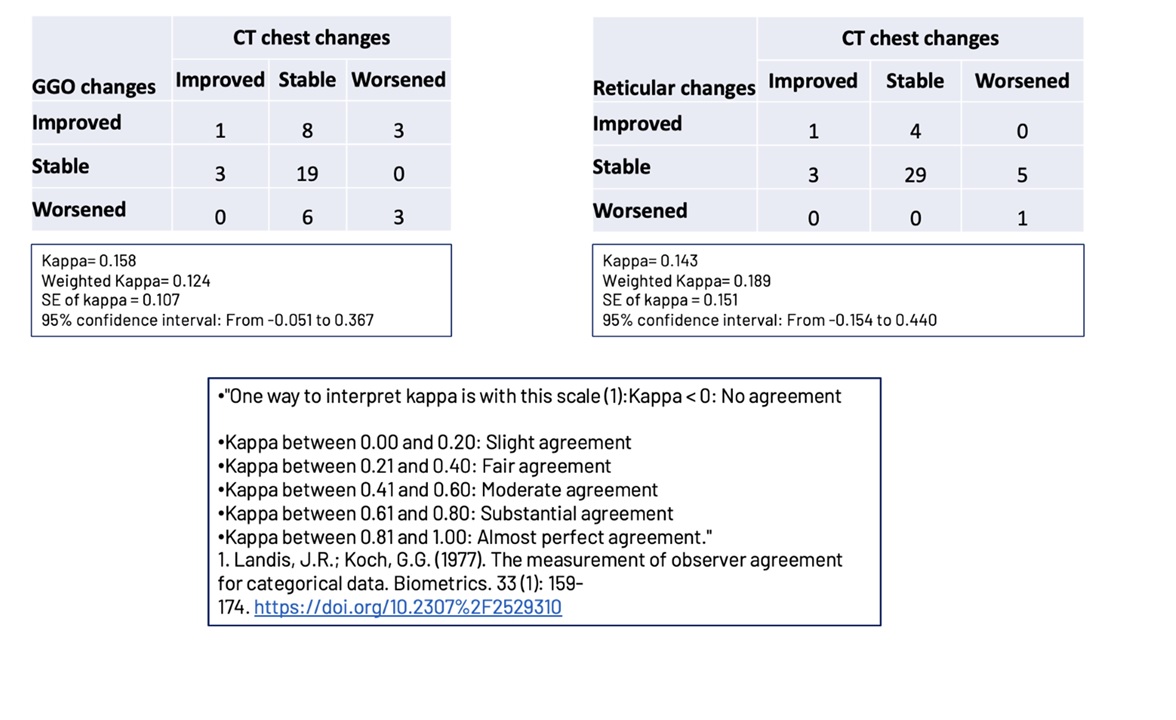
Results: Demographic and clinical characteristics of 21 patients with an average of 6 years follow-up (1-13) were included in analysis (Table 1). We had 66 HRCT and 62 PFT (FVC and DLCO), of which 52 were available for paired analysis. At baseline, HRCT was read by radiologist as GGO in 16/21 (64.8%) patients, 4/21 (19%) reticular change, 1/21(4.8%) honeycombing. CALIPER CT reported GGO in 13/21(62%) patients, 7/21 (33%) reticular change, 7/21 (48%) with PVV > 50 cm^3. Honeycombing was not detectable. Strong correlation was observed between paired CALIPER and PFT with GGO% and FVC (Spearman r = -0.71, p< 0.0001) and GGO% and DLCO (Spearman r = -0.64, p< 0.0001). Moderate correlation was seen between RP% and FVC (Spearman r = -0.39, p=0.0043) and no correlation between RP% and DLCO (Spearman r = -0.27, p=0.05) (Graph 1a). Interestingly, there was no correlation with the degree of change between CALIPER and PFT parameters (data not shown). A significant correlation was observed between annualized GGO% and annualized FVC% (Spearman r = -0.51, p=0.019) and RP% and FVC% (Spearman r = -0.45, p=0.04) (Graph 1b). There was no correlation between annualized GGO% and DLCO% or RP% and DLCO% (Graph 1b). There was no correlation between PVV and any of PFT parameters (data not shown). There was a poor agreement between change in CALIPER parameters and traditional CT chest response (Table 2).
Conclusion: In our IIM-ILD cohort, CALIPER HRCT showed strong correlation with both serial and annualized FVC and DLCO changes but had poor agreement with HRCT change as recorded by the radiologist. This suggests advantage of digital analysis over traditional HRCT in determining progression in ILD with potential to be useful for evaluating treatment response.
To cite this abstract in AMA style:
Narain S, Shargani K, Ilic I, Buttar I, Marder G. Computer Aided Lung Informatics, HRCT and PFT in Patients with Interstitial Lung Disease in Idiopathic Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/computer-aided-lung-informatics-hrct-and-pft-in-patients-with-interstitial-lung-disease-in-idiopathic-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/computer-aided-lung-informatics-hrct-and-pft-in-patients-with-interstitial-lung-disease-in-idiopathic-inflammatory-myopathies/