Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster III: Treatment
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus anticoagulant (LAC) is an established risk factor for thrombosis in systemic Lupus erythematosus (SLE). Emerging data suggest that activation of the complement system is also involved in the pathogenesis of thrombosis. Our objective was to evaluate the relationships between complement C4d split products deposited on erythrocytes (EC4d), Platelets (PC4d) and thrombosis in SLE.
Methods: This was a cross sectional analysis of 148 consented SLE patients (by ACR or SLICC criteria; 82% ANA positive [>1:80] by indirect immunofluorescence; mean age: 47±1 years, 32% taking prednisone; mean SELENA-SLEDAI: 2.5±0.2 points). SLE were classified with (n=16, 11%) or without (n=132, 89%) a history of thrombotic events (venous or arterial) in the past 5 years. EC4d and PC4d levels were measured using quantitative flow cytometry, and expressed as mean fluorescence intensity (MFI) (abnormal EC4d>14 net MFI, PC4d>20 net MFI, each corresponding to the 99th percentile of normal healthy group). Complement C3, C4 and LAC were measured using immunochemistry (low C3<81 mg/dl, low C4<12.9 mg/dl) and Dilute Russell Viper Venom Time (positive DRVVT>37 seconds), respectively. Statistical analysis consisted of Mann Whitney test and logistic regression.
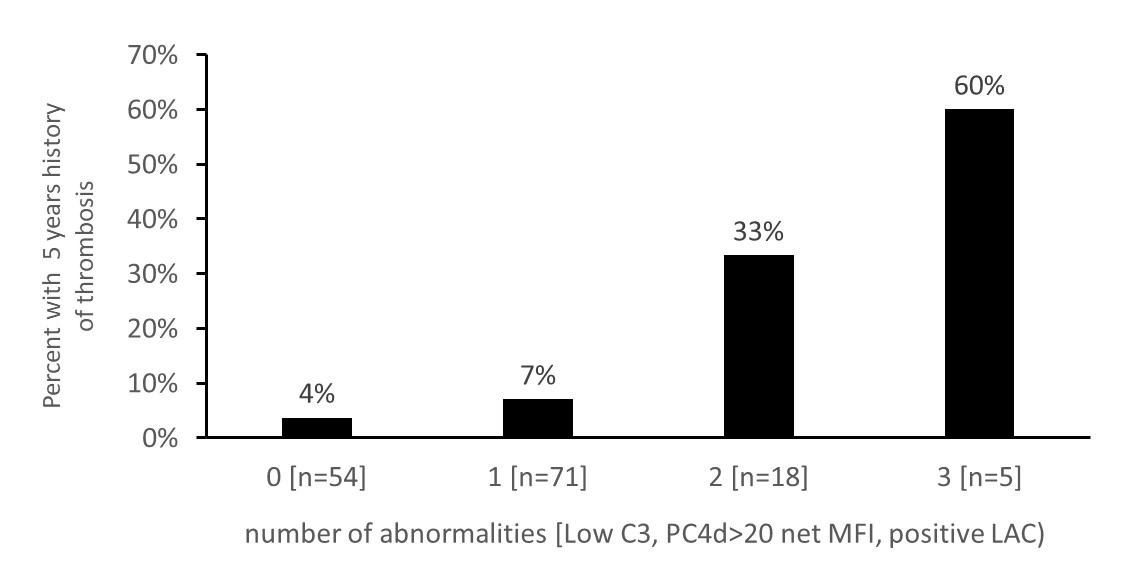
Results: SLE with a history of thrombosis in the past 5 years presented with 5.5 and 2.2-fold higher median PC4d (27 [IQR: 8-79 net MFI] vs 5 [IQR: 2-14 net MFI] net MFI) and EC4d (19 [IQR: 9-59 net MFI] vs 9 [IQR: 6-19] net MFI]) levels, respectively, than SLE without thrombotic events (p<0.001; n=148). Low C3 (OR=10.5 [CI 95%: 2.6-42.0]), low C4 (OR=3.5 [CI 95%: 1.1-11.1), abnormal PC4d (OR=19.0 [CI 95%: 3.7-96.4; n=148), EC4d (OR=4.0 [CI95%: 1.3-11.8]), and LAC (OR=5.3 [CI 95%: 1.1-24.5; n=144) were all significantly associated with thrombosis (p<0.035). Prednisone was also associated with thrombosis (OR=3.2 [CI95%: 1.1-8.9]) (p=0.037). Multivariate analysis revealed that low C3, abnormal PC4d and LAC were all independently and significantly associated with thrombosis (p<0.027) and the cumulative presence of these abnormalities resulted in higher likelihood of thrombosis (OR range: 81.9 CI95%: 9.7-688.5; n=144) (p<0.001) (Figure). These results remained significant after adjusting for prednisone.
Conclusion: Complement C4d split products associate with thrombotic events in SLE, independent of other risk factors. A composite score of risk factors performed better than single risk factors alone, and should be studied prospectively.
Disclosure: M. Petri, Exagen Diagnostics, Inc., 2; J. Conklin, Exagen Diagnostics Inc., 3; R. Apilado, Exagen Diagnostics, 3; T. O'Malley, Exagen Diagnostics, 3; J. Ligayon, Exagen Diagnostics, Inc, 3; L. Wolover, Exagen Diagnostics, Inc., 3; T. Dervieux, exagen, 3.
To cite this abstract in AMA style:
Petri M, Conklin J, Apilado R, O'Malley T, Ligayon J, Wolover L, Dervieux T. Complement C4d Split Products in Combination with Lupus Anticoagulant and Low Complement Associate with Thrombosis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/complement-c4d-split-products-in-combination-with-lupus-anticoagulant-and-low-complement-associate-with-thrombosis-in-systemic-lupus-erythematosus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/complement-c4d-split-products-in-combination-with-lupus-anticoagulant-and-low-complement-associate-with-thrombosis-in-systemic-lupus-erythematosus/