Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Lupus arthritis has heterogeneous phenotypes and severity, complicating clinical management and trial endpoints. Advances in musculoskeletal ultrasound (MSK US) and optical imaging have been proposed as objective assessment tools. In a prior study of 20 systemic lupus erythematosus (SLE) patients, we demonstrated that frequency-domain optical imaging (FDOI) and a glove-like optical imaging system (GLOIS) can differentiate inflamed from normal joints by measuring transmitted and reflected lights to assess changes in tissue properties. Here we present extended data comparing FDOI with MSK US in evaluating lupus arthritis, and exploratory findings using GLOIS to monitor arthritis resolution.
Methods: We evaluated 31 SLE patients and 22 healthy controls via convenience sampling. For each subject, 8 proximal interphalangeal (PIP) joints (bilateral PIPs 2–5) were evaluated by FDOI and MSK US within two hours. MSK US used multiplanar grey-scale (GS) and power Doppler (PD) imaging, scored by OMERACT definitions to generate a composite PDGS score. FDOI employed a 670 nm, 8 mW laser modulated at 300 MHz, and scanned across each PIP to reconstruct three-dimensional (3D) maps of light absorption and scattering. Additionally, 2 SLE patients and 2 healthy controls underwent GLOIS evaluation (Fig 1), and 1 SLE patient was evaluated by GLOIS before and after therapy for an arthritis flare. GLOIS (Fig 1) used flexible bands with 8 optical modules (each with a photodiode and 3 LEDs at 530, 660, and 880 nm). LEDs were sequentially activated; photodiodes captured the transmitted signals. A sphygmomanometer was inflated to the subject’s diastolic blood pressure, inducing a complete venous occlusion and partial arterial occlusion, then released after 60 seconds accompanied by 60 more seconds of measurement. Subsequently, the measurements from all the source/detector pairs around the finger joint were used to tomographically reconstruct the distributions of total hemoglobin (HbT) concentrations in the joint.
Results: FDOI data (Fig 2) from 235 PIPs (SLE) and 136 PIPs (controls) produced an AUC of 0.87, with 89% sensitivity and 66% specificity (Fig 2A, 2B). Among 120 joints assessed by MSK US, PDGS scores were 0 (n=47), 1 (n=73), 2 (n=61), and 3 (n=54). Joints with moderate/severe arthritis (PDGS 2–3) had significantly higher scattering (8.8±1.4 vs. 8.3±0.6/cm, p< 0.01, Fig 2C) and absorption coefficients (0.25±0.18 vs. 0.18±0.1/cm, p< 0.01, Fig 2D) than those with minimal/no inflammation (PDGS 0–1).3D tomographically reconstructed GLOIS imaging showed higher HbT concentration at pressure release (Fig 3A) and 30 seconds post-release (Fig 3B) in SLE joints (42 μM at both timepoints) with PDGS of 2 compared to controls (29 and 30 μM). In the SLE patient examined at the time of flare (T1) and after symptom resolution (T2), Fall Time AUC decreased in 4 of 6 fingers (Fig 3C), suggesting improvement.
Conclusion: These data support the use of FDOI and GLOIS to reliably detect MSK US-confirmed arthritis in SLE joints and to monitor disease activity. Optical imaging shows promise as a non-invasive, objective tool for lupus arthritis assessment in clinical care and trials. Further development is warranted and ongoing.
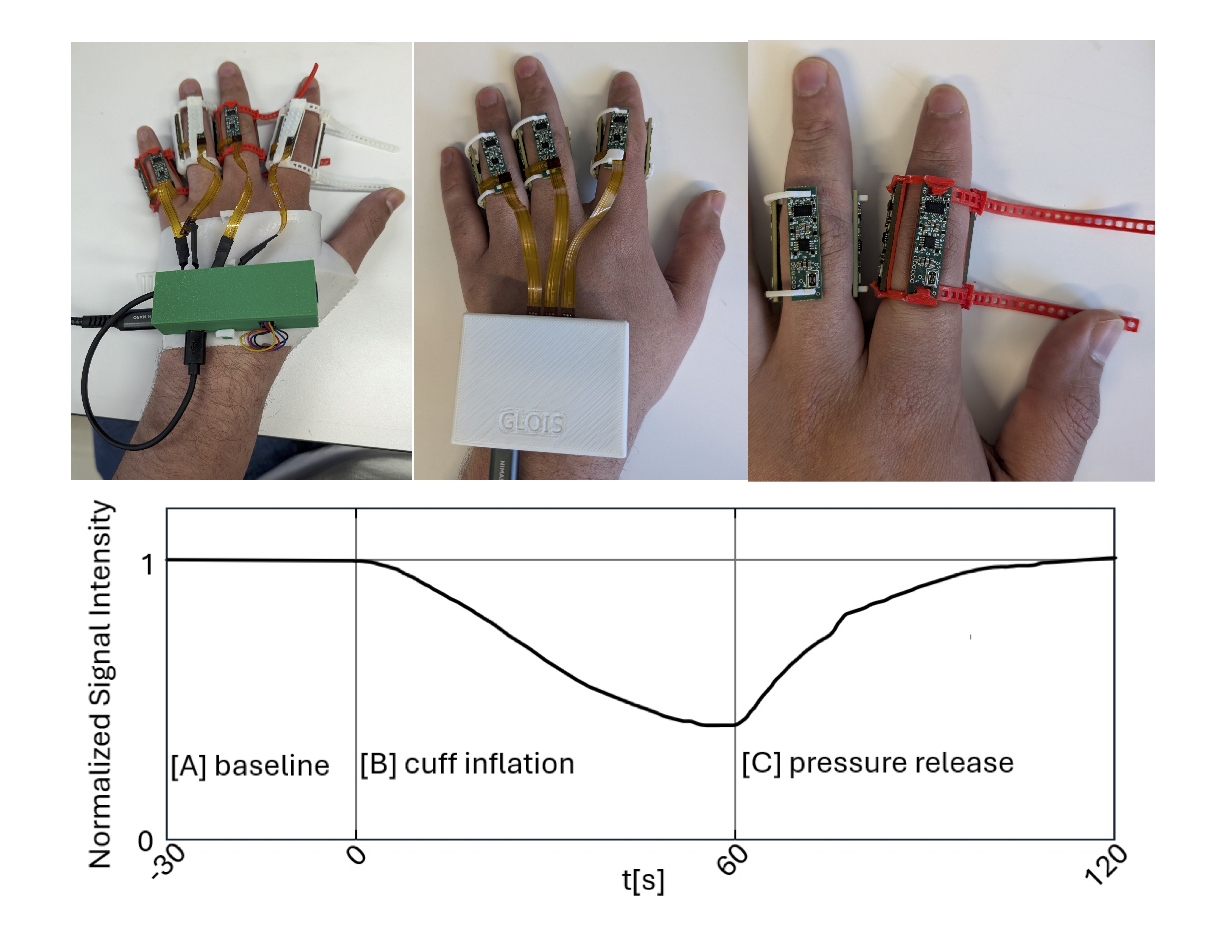 Figure 1. Glove-like optical imaging system (GLOIS) in the Evaluation of Lupus Arthritis
Figure 1. Glove-like optical imaging system (GLOIS) in the Evaluation of Lupus Arthritis
The top part of the figure exhibits the glove-like optical imaging system (GLOIS), which comprises a control module, four optical imaging patches, a flexible printed circuit (FPC) connecting band, and an adjustable flexible fixation band. The optical imaging patches deliver light into the affected joint and measure the resulting reflected and transmitted light. Each patch comprises two source-detector modules spaced 10 mm apart, each with three light-emitting diodes (LEDs) (wavelength λ = 880 nm, 660 nm, and 530 nm) and a photodiode. The patches are connected to each other and the control module via the flexible connecting band at 15 mm spacings, allowing the patches to be wrapped around the proximal inter-phalangeal (PIP) joint. The band and patches are fixed to the finger using a 3D-printed flexible fixation band.
The bottom part of the figure shows a typical signal trace measured by GLOIS for one source detector, showing significant events, including the baseline measurement (A), the sphygmomanometer cuff inflation (B) to the subject’s diastolic blood pressure causing a complete venous occlusion and partial arterial occlusion , and the release of pressure (C) accompanied by 60 more seconds of measurement.
.jpg) Figure 2. Evaluation of lupus arthritis by frequency domain optical imaging (FDOI) in comparison to musculoskeletal ultrasound (MSK US)
Figure 2. Evaluation of lupus arthritis by frequency domain optical imaging (FDOI) in comparison to musculoskeletal ultrasound (MSK US)
ROC curve (A) and discriminant linear analyses (B) of frequency domain optical imaging (FDOI) in comparison to musculoskeletal ultrasound (MSK US) evaluation of lupus arthritis. The three parameters of choice for the discriminant analysis include the mean of the scattering coefficient, variation of the absorption coefficient, and percentage of total finger volume interested.
Joints with no/minimal arthritis (PDGS 0 or 1) and moderate/severe arthritis (PDGS 2 or 3) show significantly different mean and standard error of scattering (C) and absorption (D) in reconstructed optical data.
.jpg) Fig 3. Glove-like optical imaging system (GLOIS) evaluation of joints in patients with lupus and healthy controls
Fig 3. Glove-like optical imaging system (GLOIS) evaluation of joints in patients with lupus and healthy controls
3D Reconstructions of the total hemoglobin (HbT) concentrations in a healthy subject and control subjects at the time of pressure release (A) and 30 seconds after pressure release (B). AUC of Fall Time decreases for 4 of the 6 fingers (C) during and after a lupus arthritis flare.
To cite this abstract in AMA style:
Tang W, Rosas Chavez G, Khalili L, Nordmann-Gomes A, Suh S, Marone A, Bardien M, Kim S, Geraldino-Pardilla L, Hielscher A, Askanase A. Comparison of Optical Imaging with Musculoskeletal Ultrasound in Assessment of PIP Joints of Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/comparison-of-optical-imaging-with-musculoskeletal-ultrasound-in-assessment-of-pip-joints-of-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-optical-imaging-with-musculoskeletal-ultrasound-in-assessment-of-pip-joints-of-systemic-lupus-erythematosus-patients/
