Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Eosinophilic granulomatosis with polyangiitis (EGPA) is a rare vasculitis marked by asthma and eosinophilia, often leading to severe, persistent respiratory symptoms. Unlike severe asthma without EGPA, patients with EGPA typically have longstanding asthma prior to vasculitis onset and show widespread eosinophilic inflammation. These differences necessitate distinct treatment approaches. This study compares the demographic and clinical characteristics of patients with severe asthma with and without EGPA using data from the National Inpatient Sample Database.
Methods: A retrospective cross-sectional study was conducted using data from NIS (2016 to 2021). Primary and secondary diagnoses were identified using International Classification of Diseases (ICD-10) codes. All patients aged >18 years with severe asthma were included in the study. Patients were divided into two groups: those with severe asthma and EGPA (n=775) and those with severe asthma without EGPA (n=201,765). Demographics, hospital region, comorbidities, complications, and outcomes, including mortality, length of stay, and hospitalization charges, were compared between the 2 groups. Statistical analysis was done using STATA v.17.
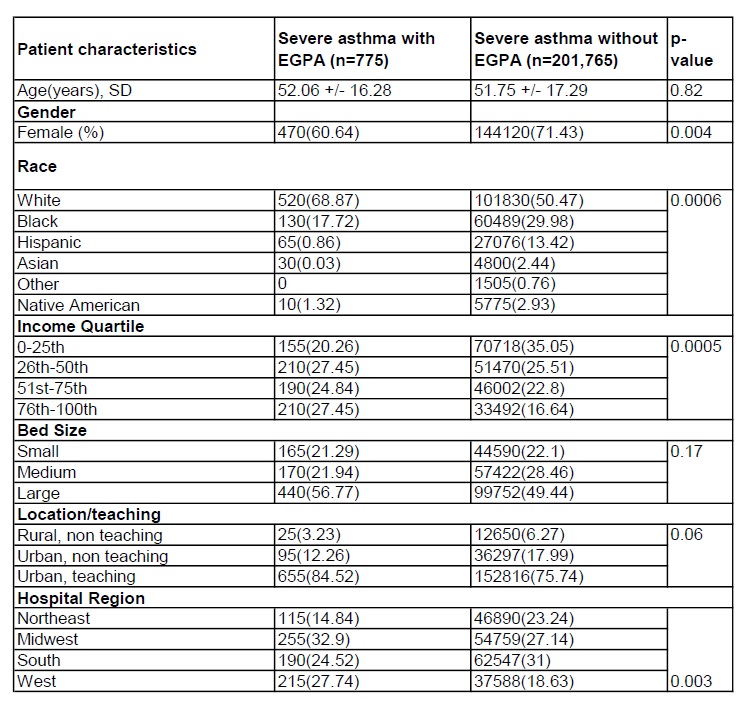
Results: The mean age of patients with severe asthma and EGPA was 52.06 years compared to 51.75 years in those without EGPA (p=0.82). A significantly lower proportion of females was observed in the EGPA group (60.64%) compared to the non-EGPA group (71.43%) (p=0.004). In the EGPA group, there was a higher percentage of White patients (68.87% vs. 50.47%) and a lower percentage of African American patients (17.72% vs. 29.98%). A higher proportion of EGPA patients were treated in urban teaching hospitals (84.52% vs. 75.74%, p=0.06). Comorbidities such as diabetes (8.39% vs. 19.24%, p=0.0006) and chronic obstructive pulmonary disease (5.81% vs. 12.18%, p=0.01) were less common in the EGPA group. However, the incidence of acute myocardial infarction (10.97% vs. 5.5%, p=0.002) was higher in the EGPA group. Notably, there was no significant difference in terms of complications like pneumothorax, acute respiratory failure and mechanical ventilation. There were no statistically significant differences in the outcomes, including mortality, hospital stay, and total costs, between the 2 groups.
Conclusion: This study demonstrates that patients hospitalized with severe asthma and concomitant eosinophilic granulomatosis with polyangiitis (EGPA) exhibit distinct demographic and clinical profiles compared to those without EGPA. Importantly, the presence of EGPA does not appear to increase the risk of acute respiratory complications such as pneumothorax, acute respiratory failure, or the need for mechanical ventilation. Moreover, no significant differences were observed in key hospital outcomes—including mortality, length of stay, or total hospitalization costs. These findings suggest that although EGPA defines a unique subset within the severe asthma population, it does not independently contribute to worse short-term inpatient outcomes.
.jpg) Table 2: Co-morbidities and Complications
Table 2: Co-morbidities and Complications
To cite this abstract in AMA style:
Subedi P, Regmi A, Shrestha K, Ghimire M, Poudel S, Ghimire K, Pandey O, Tagoe C. Comparison of Demographics and Outcomes of Inpatient Hospitalization of Severe Asthma Patients with Eosinophilic Granulomatosis with Polyangitis. A Study on the National Inpatient Sample Database [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/comparison-of-demographics-and-outcomes-of-inpatient-hospitalization-of-severe-asthma-patients-with-eosinophilic-granulomatosis-with-polyangitis-a-study-on-the-national-inpatient-sample-database/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-demographics-and-outcomes-of-inpatient-hospitalization-of-severe-asthma-patients-with-eosinophilic-granulomatosis-with-polyangitis-a-study-on-the-national-inpatient-sample-database/

.jpg)