Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Similar to nailfold videocapillaroscopy (NVC), automated capture and analysis of sublingual microvessel segments (intravital microscopy) can define vasculopathy, and distinguish systemic sclerosis (SSc) patients from healthy controls. The aim of this study is to compare automated capture and analysis of sublingual microcirculation parameters with NVC derived scores for assessment of SSc-related vasculopathy.
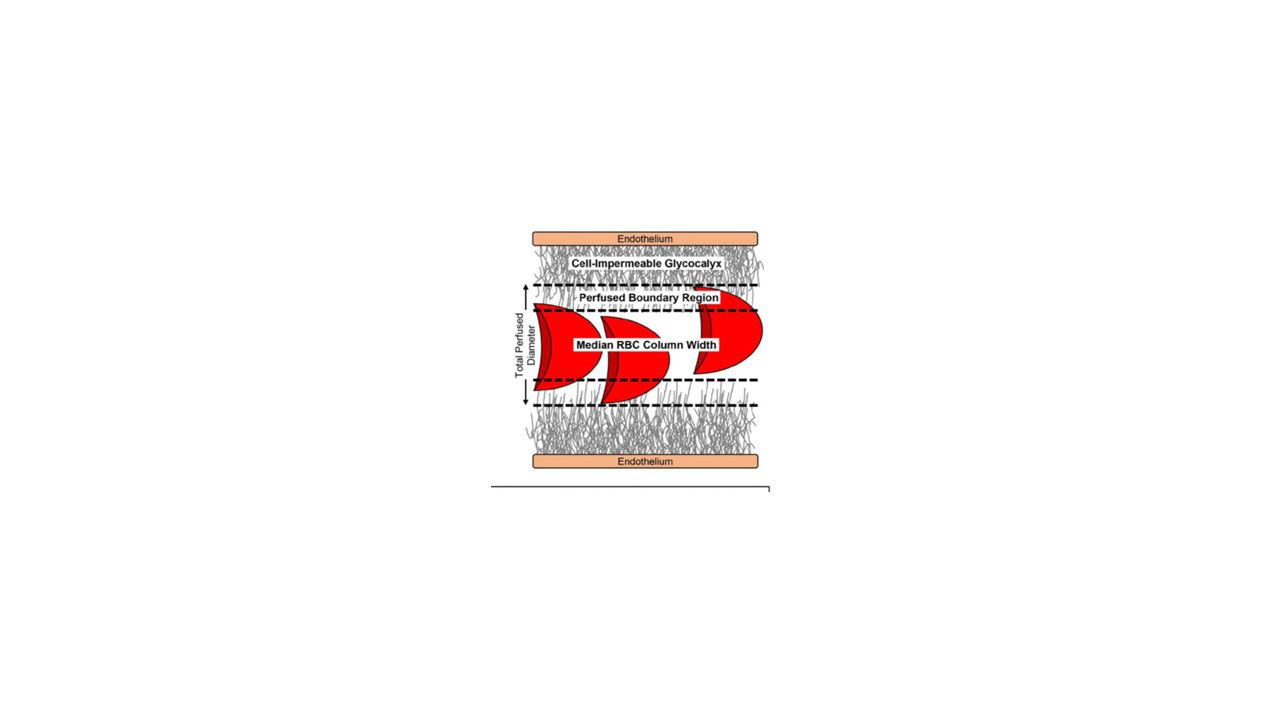
Methods: Consecutive, consented SSc registry patients that met ACR/EULAR classification criteria had intravital microscopy of the sublingual microcirculation and NVC at the time of routine care. The following intravital microscopy parameters were captured: total microvascular density, median RBC width (RBCfract) and perfused boundary region (PBR) (Figure 1). The following NVC parameters were obtained: (1) capillaroscopy patterns (early, active and late); (2) degree of enlarged capillaries, giant capillaries, capillary hemorrhages, capillary density, disorganization of vascular array and capillary ramification assessed by a semi-quantitative method; and (3) microangiopathy evolution score (sum of capillary density, disorganization of vascular array and capillary ramification). Non-parametric tests were used for statistical evaluation.
Results: Thirty-nine SSc patients were enrolled (37 women and 2 men, mean age 59±21 years, mean SSc duration years 9.5±8.9, 30 limited cutaneous SSc and 9 diffuse cutaneous SSc). There was a statistically significant negative correlation between sublingual total microvascular density and microangiopathy evolution score (r=-0.532, p=0.0006). Furthermore, there was a highly significant inverse association between the total microvascular density and number of capillaries measured by NVC (r=-0.569, p=0.0002). There was significant, negative correlation between the total microvascular density and disorganization of vascular array and capillary ramification (r=-0.461, p=0.003) and degree of giant capillaries (r=-0.387, p=0.01). There was no correlation between RBCfract and PBR with NVC parameters.
Conclusion: This study confirmed a significant correlation between intravital microscopy of the sublingual microcirculation and NVC in terms of sublingual total microvascular density and microangiopathy evolution score. The two methods did not correlate in all captured parameters. Consequently, in order to define progressive vasculopathy in SSc, intravital microscopy of the sublingual microcirculation could be a valuable tool in addition to NVC for longitudinal analysis.
To cite this abstract in AMA style:
Radic M, Thomas J, Frech T. Comparison of Automated Capture and Analysis System of Sublingual Microvessels and Nailfold Videocapillarscopy for Microvascular Assessment in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparison-of-automated-capture-and-analysis-system-of-sublingual-microvessels-and-nailfold-videocapillarscopy-for-microvascular-assessment-in-systemic-sclerosis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-automated-capture-and-analysis-system-of-sublingual-microvessels-and-nailfold-videocapillarscopy-for-microvascular-assessment-in-systemic-sclerosis/