Session Information
Session Type: ACR Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Current classification criteria differentiate between Takayasu’s arteritis (TAK) and giant cell arteritis (GCA), the two most common forms of large-vessel vasculitis, based primarily on clinical assessment, yet patients with TAK and GCA may differ in patterns of arterial disease. This study aimed to use computer-based algorithms to determine if patterns of arterial disease are useful to differentiate TAK from GCA with large-vessel involvement (LV-GCA).
Methods: Patients with TAK or LV-GCA were studied from four independent cohorts: a large, international cohort and three separate cohorts combined into one North America cohort. Case inclusion required evidence of large-vessel involvement, defined as stenosis, occlusion, or aneurysm by imaging or catheter-based angiography or ultrasound, or increased FDG uptake by positron-emission tomography (PET) in at least one of 11 specified arterial territories. K-means cluster analysis was performed to identify clusters of patients based on pattern of arterial involvement. Cluster groups were identified in the international cohort and independently validated in the combined North American cohort.
Results: A total of 1,068 patients were included (International: TAK=461, GCA=217; NA: TAK=225, GCA=165). Patients with TAK underwent angiography (95%), ultrasonography (28%), and/or PET imaging (14%). Patients with LV-GCA underwent angiography (50%), ultrasonography (52%), and/or PET imaging (58%). Six distinct clusters of patients were identified in the international cohort and validated in the North American cohort (Figure). Patients in Clusters One, Two, and Three were significantly more likely to have TAK, and patients in Clusters Four, Five, and Six were significantly more likely to have LV-GCA. Out of all study patients, involvement of the abdominal aorta and renal/mesenteric arteries was the most specific pattern for TAK (TAK: 134 (92%) vs GCA: 11 (8%), p< 0.01), while bilateral subclavian/axillary disease was the most specific pattern for GCA (GCA: 92 (80%) vs TAK: 23 (20%), p< 0.01). Among patients who underwent both angiography and PET, patients with TAK were more likely than patients with GCA to have damage by angiography without associated inflammation by PET (TAK: 52% vs GCA: 7%, p< 0.001), and patients with GCA were more likely than patients with TAK to have arterial FDG-uptake by PET without associated vascular damage (GCA: 80% vs TAK: 23%, p< 0.001).
Conclusion: These findings support the incorporation of arterial patterns of disease into classification criteria for large-vessel vasculitis and highlight shared and divergent vascular phenotypes between TAK and GCA.
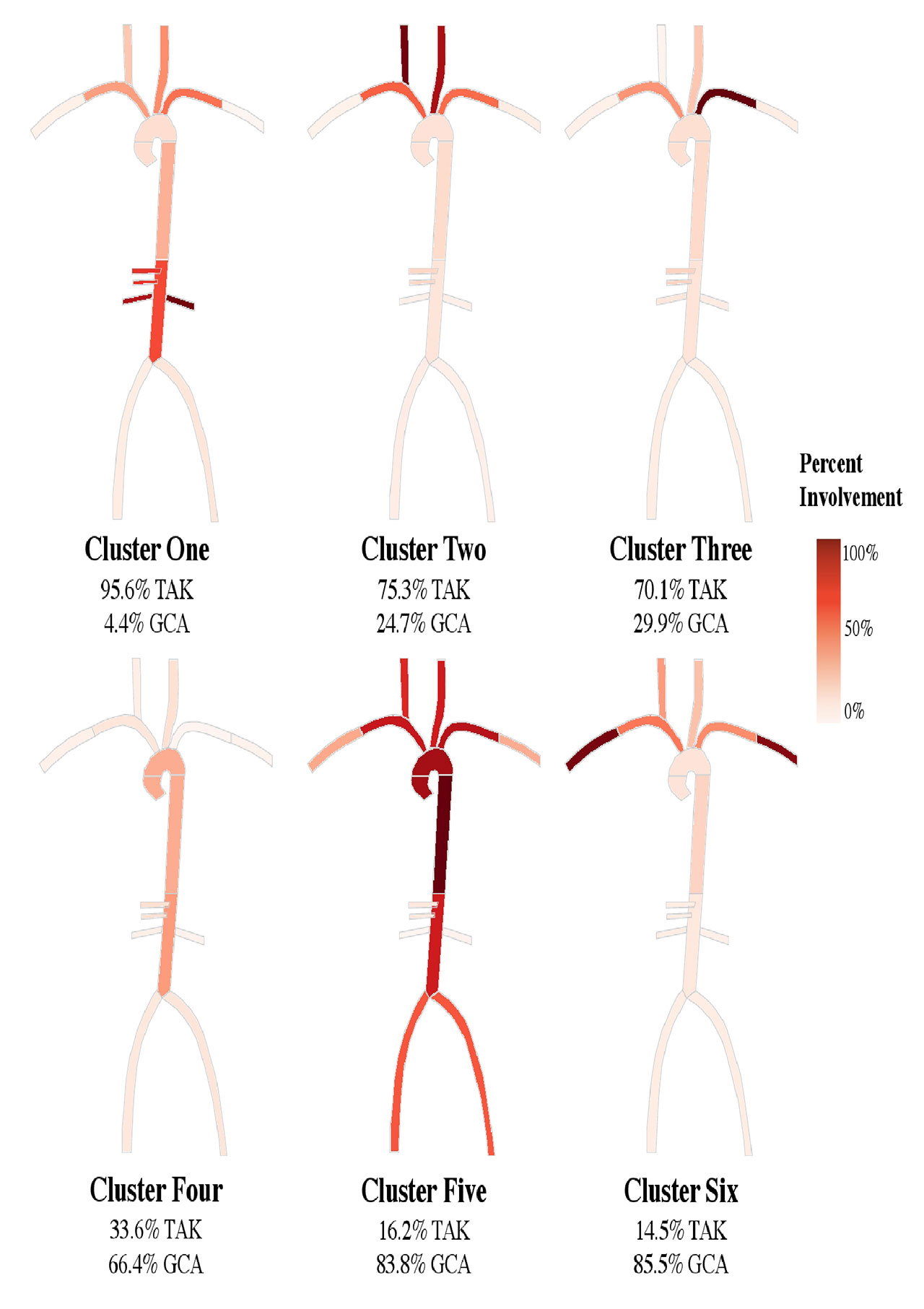
2019.03.14 TAK and GCA Imaging – Figures
To cite this abstract in AMA style:
Gribbons K, Ponte C, Craven A, Cuthbertson D, Carette S, Hoffman G, Khalidi N, Koening C, Langford C, Maksimowicz-McKinnon K, McAlear C, Monach P, Moreland L, Pagnoux C, Quinn K, Robson J, Seo P, Sreih A, Suppiah R, Warrington K, Ytterberg S, Luqmani R, Watts R, Merkel P, Grayson P. Comparison of Arterial Patterns of Disease in Takayasu’s Arteritis and Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparison-of-arterial-patterns-of-disease-in-takayasus-arteritis-and-giant-cell-arteritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-arterial-patterns-of-disease-in-takayasus-arteritis-and-giant-cell-arteritis/
