Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: As shown in previous studies, outcomes in SLE are affected by social determinants of health which influence health care disparities. Evaluating health disparities through the lens of spatial context is an evolving field. Various indices have been developed to categorize the vulnerability of an area. Two such measures are the Center for Disease Control Social Vulnerability Index (SVI) and the Area Deprivation Index (ADI) by the University of Wisconsin-Madison. SVI was created with the intention of identifying vulnerable areas in times of disaster, while ADI was specifically created to inform healthcare delivery in disadvantaged neighborhoods. In addition, SVI is reported by census tract, versus ADI which is reported by census block (subdivision of census tract). Given the difference in intention behind each index and difference in area studied, we sought to understand whether SVI and ADI would have consistent associations with SLE disease activity and prednisone utilization. We also hypothesized that prednisone overutilization is prevalent across vulnerability indices, and that differences in prednisone use will be seen even between neighborhoods.
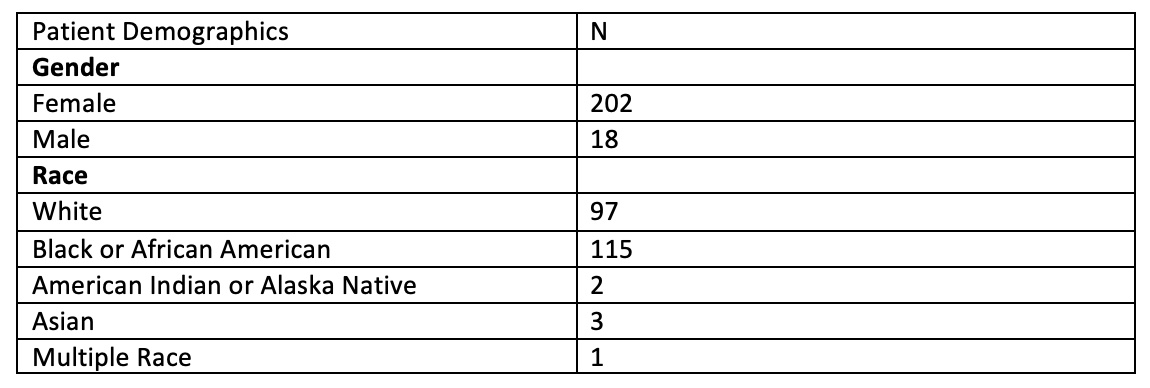
Methods: Patients from the Washington University Lupus Center who met either ACR or SLICC classification criteria for SLE were longitudinally assessed from April 2014 to August 2020. The patient’s census tract and census block were determined using the address listed for each patient’s index visit. Only patients with available SVI, ADI, disease activity assessments (SLEDAI 2000 Responder Index-50, S2K RI-50), and prednisone dose data were included. Census tracts corresponded to SVI from the CDC database, and census blocks corresponded to ADI from the Neighborhood Atlas. SVI ranges from 0 to 1, with 1 being most socially vulnerable, while ADI ranges from 0 to 100 with the 100th percentile being most disadvantaged. Any patient living in an area above the mean of 0.5 or 50th percentile can be seen as living in a socially vulnerable or disadvantaged area. SLE disease activity was assessed using the S2K RI-50, where scores > 4 correlated with active SLE. Prednisone prescribed at the index visit was divided into 4 categories (none, 0-7.5 mg, 8-20 mg, >20 mg).
Results: 220 patients were analyzed. There was no significant correlation between cumulative SVI and disease activity (OR 1.09, 95% CI=0.607-1.975, p=0.7635). Patients living in more disadvantaged areas per ADI were more significantly likely to have active disease (OR 1.65, 95% CI=0.864-3.161, p=0.129), although this was not statistically significant. Both those with vulnerable cumulative SVI (OR 2.23, 95% CI=1.24-3.99, p=0.006) and disadvantaged ADI were also more likely to be prescribed higher doses of prednisone (OR 3.57, 95% CI=1.73-7.36, p=0.0002).
Conclusion: Patients living in vulnerable areas determined by either SVI or ADI are likely to be prescribed higher doses of prednisone, despite having no statistically significant correlation with disease activity. This strongly suggests that those in more vulnerable or disadvantageous areas leverage prednisone utilization to control disease activity, which we hypothesize worsens long-term outcomes for this population.
To cite this abstract in AMA style:
Som A, McMorrow L, Chen L, Sen D, Baker E, Kim A. Comparing Social Vulnerability Index to Area Deprivation Index to Patient Outcomes in SLE and Glucocorticoid Utilization [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/comparing-social-vulnerability-index-to-area-deprivation-index-to-patient-outcomes-in-sle-and-glucocorticoid-utilization/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparing-social-vulnerability-index-to-area-deprivation-index-to-patient-outcomes-in-sle-and-glucocorticoid-utilization/