Session Information
Date: Tuesday, October 28, 2025
Title: (2052–2078) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Studies of idiopathic inflammatory myopathies (IIM) are often based on the analysis of single cohorts at academic centers. We aimed to identify potential gaps in care by comparing testing, treatment, and outcomes of people with IIM diagnosed as dermatomyositis (DM) vs polymyositis (PM) in a nationally representative US cohort.
Methods: This retrospective cohort study used commercial claims (Komodo Healthmap data 1/1/2016-3/31/2024) to identify adults ≥18 with incident IIM, requiring one inpatient diagnosis code for DM (M33.1* or M33.9*) or PM (M33.2*) (positive predictive value 92%) or two outpatient diagnosis codes for DM or PM 7-365 days apart with use of a non-glucocorticoid immunomodulatory therapy (second outpatient diagnosis as the index date). Patients without a 12-month baseline prior to diagnosis #1 or with diagnoses of juvenile DM or inclusion body myositis were excluded. Antisynthetase syndrome and necrotizing myopathy lack specific codes but could be included if DM or PM diagnoses were coded. Standardized differences ≥|0.1| were used to identify differences between those with DM vs PM. Analyses of diagnostic testing and treatment required 12 months of continuous data after index unless limited by death. Time to event analyses for incident hospitalization and major adverse cardiac events (MACE, excluding those with prior MACE) censored at end of follow-up.
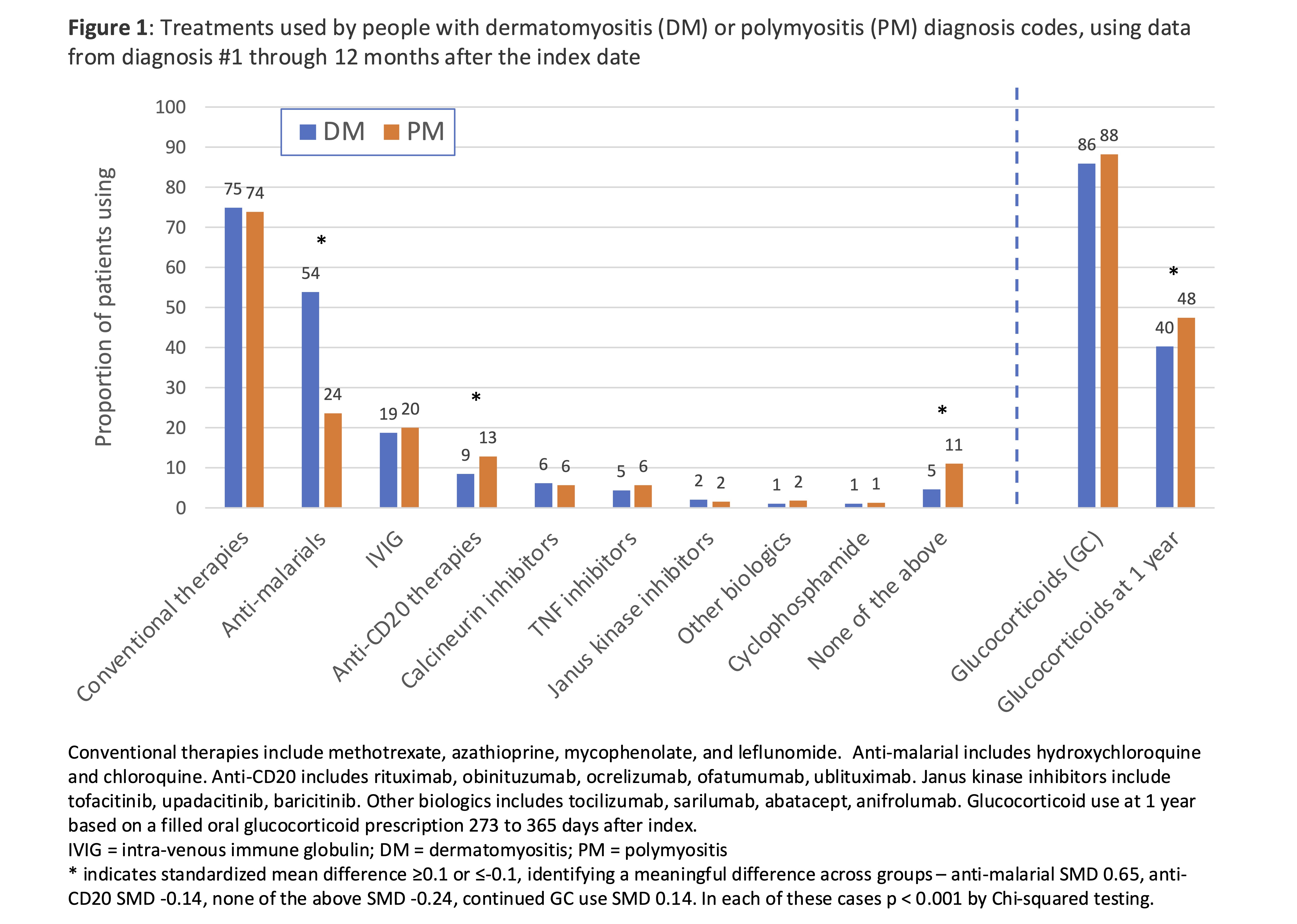
Results: We identified 9,195 people with incident IIM: 5,560 with DM and 3,635 with PM. People with DM were younger, more frequently female, had fewer comorbidities, and were less often diagnosed as inpatients vs PM (Table 1). Other rheumatic diagnoses were common in both groups, and those with PM were more likely to have prior diagnoses of rhabdomyolysis or abnormal liver function tests (possibly reflecting muscle injury not identified as IIM). Rheumatologists cared for approximately 70% of those with DM and PM, with dermatologists more frequently involved for DM and neurologists and cardiologists for PM (Table 2). Although 19% of patients had a diagnosis of ILD, no pulmonary testing was performed in 35% of patients. Conventional therapies were frequent in both groups, but anti-malarials were used more commonly in those with DM (Figure 1). IVIG (19%) and anti-CD20 therapy (10%) use in the first year was not uncommon in DM or PM. Glucocorticoid use was similar in DM and PM, with 87% using glucocorticoids within the first year of diagnosis and median cumulative glucocorticoid exposure among glucocorticoid users 1605mg (IQR 600, 2925). Glucocorticoid use at 1 year, however, was less common in DM (40%) vs PM (48%). During follow-up, incidence of hospitalization (15.1 vs 22.1/100 person-year) and MACE (1.0 vs 1.7/100 person-years) were less common in DM vs PM (both p < 0.05).
Conclusion: This large cohort study reveals differences in comorbidity burden and outcomes in people with DM vs PM and highlights differences in the subspecialists caring for these two populations. We found potential gaps in testing, including low rates of ILD screening. The substantial glucocorticoid burden demonstrates the need for more effective treatment.
To cite this abstract in AMA style:
George M, Riley T, Romich E, Holladay E, Beukelman T, Daigle S, Mudano A, Xie F, Guo X, Kulisek N, Yndestad A, Chaudhary A, Curtis J. Comparing characteristics, diagnostics, and treatment in people with different idiopathic inflammatory myopathies using a large representative cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/comparing-characteristics-diagnostics-and-treatment-in-people-with-different-idiopathic-inflammatory-myopathies-using-a-large-representative-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparing-characteristics-diagnostics-and-treatment-in-people-with-different-idiopathic-inflammatory-myopathies-using-a-large-representative-cohort/

.jpg)
.jpg)