Session Information
Date: Saturday, November 12, 2022
Title: Health Services Research Poster I: Lupus, RA, Spondyloarthritis and More
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Chronic inflammatory diseases have been associated with an increased risk of Alzheimer’s disease (AD), yet emerging research in rheumatoid arthritis (RA) and psoriasis suggests disease and therapy might be associated with risk of AD.1,2 Examining the relative population burden of AD in patients with various inflammatory diseases can provide valuable insight into inflammatory risk factors and potential impacts of associated therapeutics. We examined the relative 2-year incidence and prevalence of AD in patients with RA, psoriasis or psoriatic arthritis (Ps/A), inflammatory bowel disease (IBD), systemic lupus erythematosus (SLE) and other Medicare beneficiaries.
Methods: In this cohort study, we analyzed a 20% national sample of US Medicare patients from 2013-2015 to evaluate the risk of AD in each inflammatory subgroup compared to other beneficiaries without these conditions or asthma. Inclusion criteria included age ≥18 years, survival into 2014, and ≥12 months of Medicare A and B coverage. AD was identified by Medicare Chronic Condition flags in the Master Beneficiary File ( >1 International Classification of Diseases -9 or -10 codes of 331.0 or G30.0) and inflammatory subgroups using a one year baseline. Data were analyzed using multivariable logistic regression analysis and adjusted for age, sex, and race-ethnicity to calculate adjusted odds ratios and 95% confidence intervals (CI).
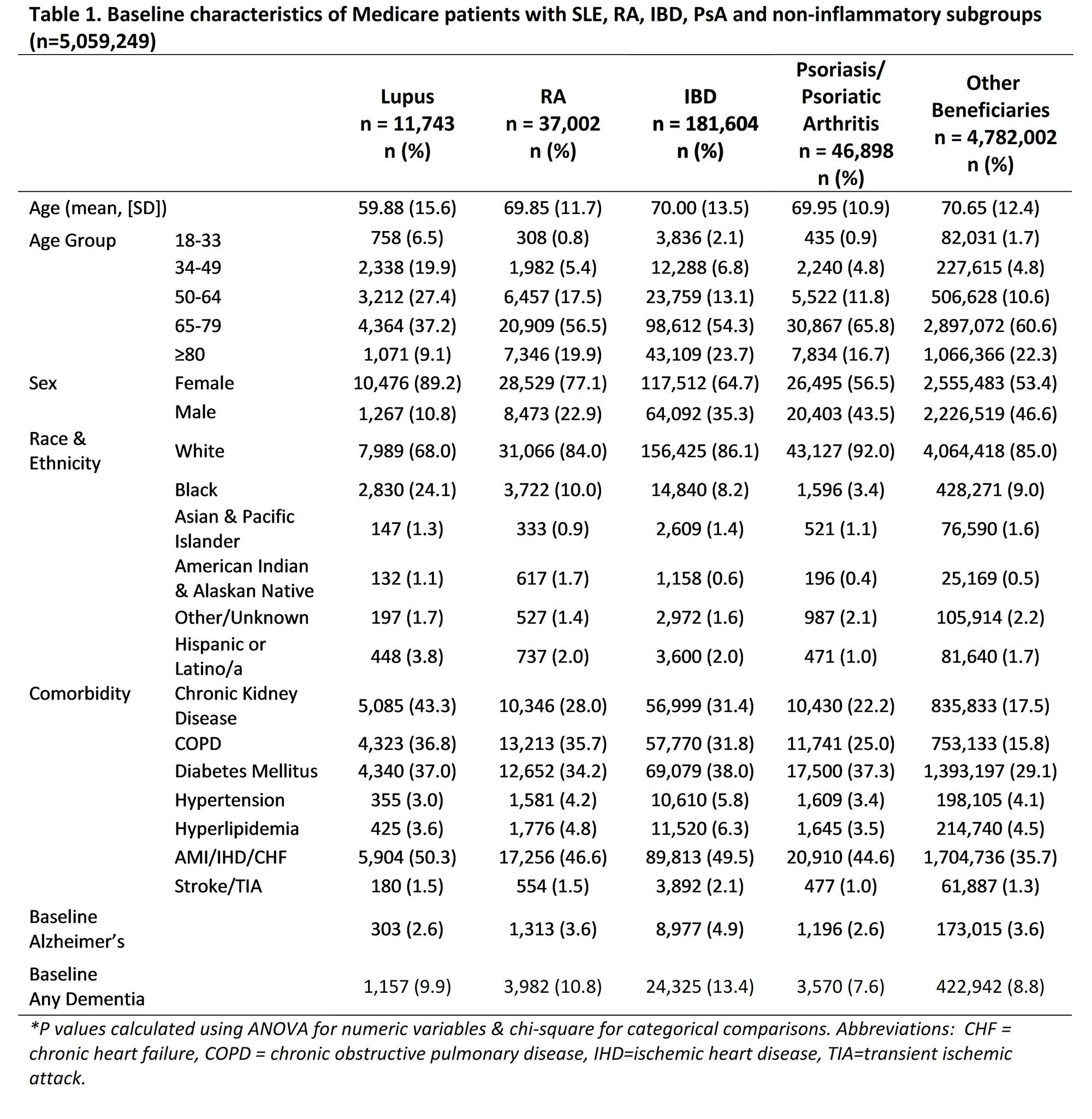
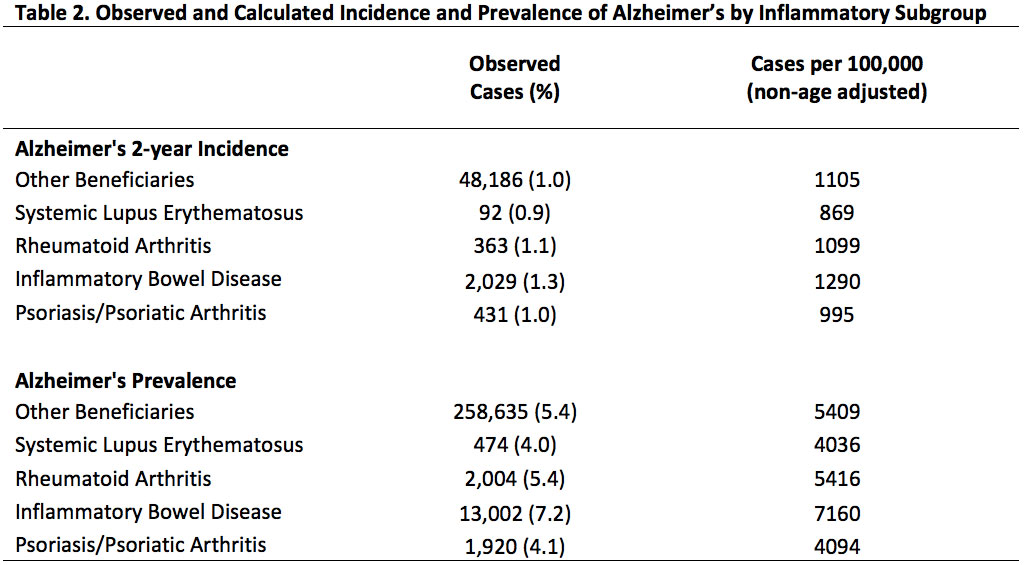
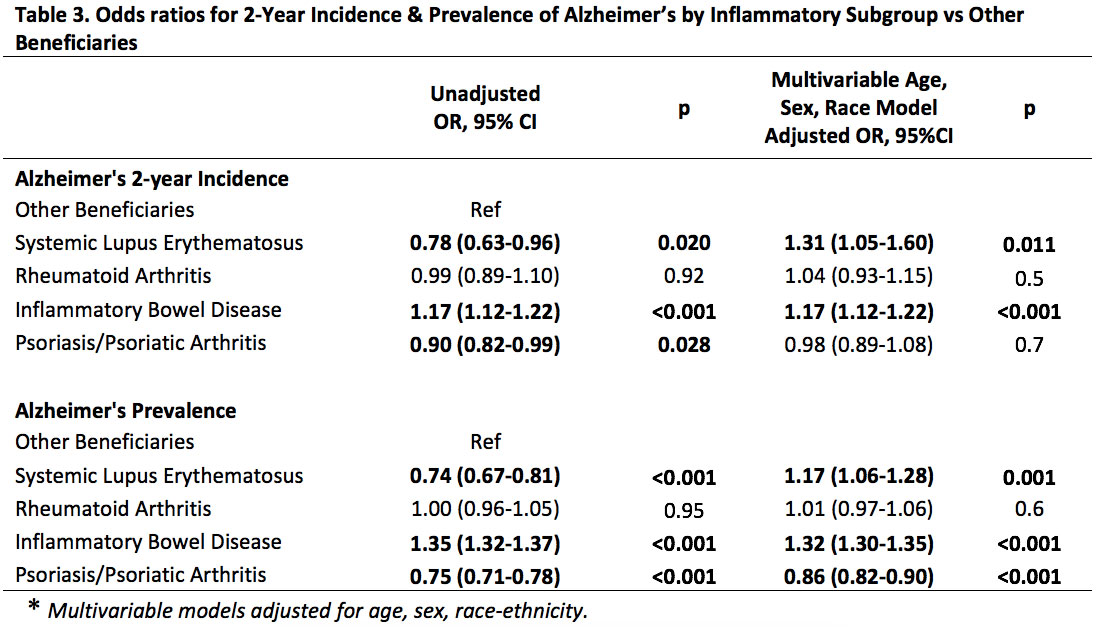
Results: Among 5,059,249 Medicare patients, we compared non-overlapping SLE (n=11,743), RA (n= 37,002), IBD (n=181,604), Ps/A (n=46,898) to other beneficiaries (n= 4,782,002). Baseline characteristics are reported in Table 1. Notably, SLE patients were a decade younger, more often female, and twice as often Black. Table 2 shows highest 2-year AD incidence and prevalence rates in IBD before age adjustment. In adjusted models, SLE and IBD associated with a higher risk of 2-year AD incidence (adjusted OR 1.31, CI 1.05-1.60 and 1.17, CI 1.12-1.22, respectively, Table 3). In Ps/A and RA, AD incidence did not differ from others.
In prevalence analysis, SLE and IBD showed the strongest odds ratios for AD (adjusted OR 1.17, CI 1.06-1.28, and 1.32, CI 1.30-1.35, respectively; Table 3). Adjusted risk of AD in RA was not statistically different, yet Ps/A had a significant negative association with AD prevalence (adjusted OR 0.86, CI 0.82-0.90; Table 3).
Conclusion: SLE and IBD subgroups were associated with a 17-32% higher risk of AD incidence and prevalence compared to other beneficiaries. Ps/A showed a 14% lower AD prevalence possibly reflecting coding differences or a potential protective treatment effect. Data suggest heightened risk of AD with SLE and IBD, which are chronic inflammatory diseases known for high levels of inflammation and steroid use. Limitations include lack of treatment data or comorbidity adjusted models. Future studies should investigate roles of inflammatory pathophysiology, comorbidity, and treatments, including anti-TNF and steroids.
References
1. Zhou M, et al.TNF blocking agents are associated with lower risk for Alzheimer’s disease…PloS One. 2020;15(3):e0229819.
2. Desai R, et al. Comparative Risk of Alzheimer Disease and Related Dementia… JAMA Netw Open. 2022;5(4):e226567.
To cite this abstract in AMA style:
Levinson J, Katz J, Chen Y, Powell W, Gilmore-Bykovskyi A, Kind A, Bartels C. Comparing Alzheimer’s Disease Risk in Patients with Chronic Inflammatory Autoimmune Diseases: A Medicare Cohort Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/comparing-alzheimers-disease-risk-in-patients-with-chronic-inflammatory-autoimmune-diseases-a-medicare-cohort-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparing-alzheimers-disease-risk-in-patients-with-chronic-inflammatory-autoimmune-diseases-a-medicare-cohort-study/