Session Information
Date: Sunday, November 12, 2023
Title: Abstracts: Metabolic & Crystal Arthropathies – Basic & Clinical Science
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: Sodium-glucose cotransporter-2 inhibitors (SGLT2i) lower serum urate (primary prevention); however, whether this translates into preventing recurrent flares among gout patients (secondary prevention) and gout-primary emergency department visits or hospitalizations remains unknown. Furthermore, their potential role on cardiovascular risk has not been studied.Our objective was to compare gout flares and cardiovascular (CV) events among gout patients initiating SGLT2i versus dipeptidyl peptidase 4 inhibitors (DPP-4i), another second-line glucose-lowering agent not associated with serum urate lowering or CV risk.
Methods: This new-user, active comparator cohort study used administrative health data covering nearly all residents of British Columbia, Canada from Jan 2014 to June 2022, including all dispensed prescriptions, regardless of funder. Primary outcome was recurrent gout flare counts, ascertained by emergency department (ED), hospitalization, outpatient, and medication dispensing records (PPV 95% for ≥ 1 flare over a similar period). We also specifically investigated flares requiring hospitalization or ED visit, and stratified by sex, age, diuretic and urate-lowering therapy (ULT) use, and gout intensity (presence of ≥1 gout-coded encounter or colchicine dispensing over the past year). Myocardial infarction and stroke were secondary outcomes. We also assessed genital infection as positive control and osteoarthritis encounter as negative control. Poisson and Cox proportional hazards regressions were used with 1:1 propensity-score matching (primary analysis) and overlap weighting (sensitivity analysis).
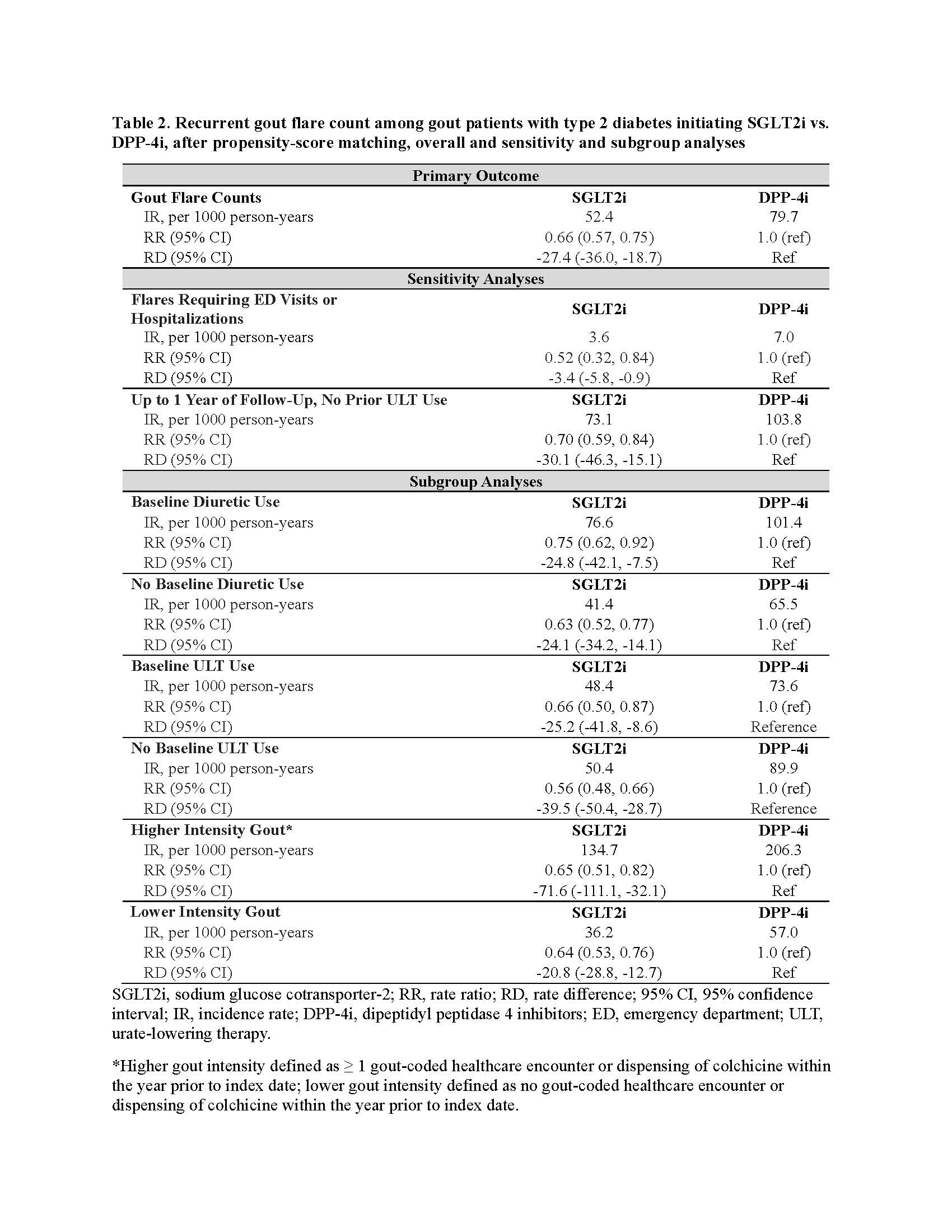
Results: We included 8150 gout patients with type 2 diabetes whose characteristics, including baseline flare rate and gout medication use, were well balanced after propensity matching (standardized mean difference< 0.1) (Table 1). During follow-up, flare rate was lower among SGLT2i initiators than DPP4i initiators (52.4 and 79.7 events per 1000 person-years, respectively), with rate ratio (RR) for SGLT2i initiation 0.66 (95% CI: 0.57, 0.75) and rate difference (RD) of -27.4 (-36.0, -18.7) fewer flares per 1000 person-years (Table 2).RR and RD for flares requiring hospitalization or ED visit were 0.52 (0.32, 0.84) and -3.4 (-5.8, -0.9), respectively. Findings were similar during the first year of SGLT2i initiation (among those without prior ULT use), suggesting no apparent paradoxical flares (Table 2). Results were consistent across subgroups, though absolute RD was higher in patients with greater gout intensity: -71.6 [-111.1, -32.1] vs. 20.8 [-28.8, -12.7] per 1000 person-years, respectively (Table 2). Hazard ratio (HR) and RD for myocardial infarction were 0.69 (0.54, 0.88) and -7.6 (-12.4, -2.8) per 1000 person-years; HR, 0.81 (0.62, 1.05) for stroke. For control outcomes, SGLT2i initiators showed higher risk of genital infection, as expected, and no altered risk of osteoarthritis encounter (Table 3).Results were similar when applying propensity-score overlap weighting.
Conclusion: Among gout patients, SGLT2i may reduce recurrent flares and gout-primary ED visits/hospitalizations, along with cardiovascular benefits, without apparent paradoxical flares.
*SMD, standardized mean difference, difference < 0.1 indicates negligible differences. ‡Frequency during the past 1 year. n, number; y, years; SD, standard deviation; SGLT2i, sodium glucose cotransporter_2 inhibitors; DPP_4i, dipeptidyl peptidase 4 inhibitors; NSAIDs, non-steroidal anti-inflammatory drugs; PPIs, proton pump inhibitors; GLP1-RA, glucagon-like peptide_1 receptor agonists.
SGLT2i, sodium glucose cotransporter_2; RR, rate ratio; RD, rate difference; 95% CI, 95% confidence interval; IR, incidence rate; DPP_4i, dipeptidyl peptidase 4 inhibitors; ED, emergency department; ULT, urate-lowering therapy.
*Higher gout intensity defined as ≥ 1 gout-coded healthcare encounter or dispensing of colchicine within the year prior to index date; lower gout intensity defined as no gout-coded healthcare encounter or dispensing of colchicine within the year prior to index date.
SGLT2i, sodium glucose cotransporter_2 inhibitors; IR, incidence rate; HR, hazard ratio; RD, risk difference; DPP_4i, dipeptidyl peptidase 4 inhibitors; 95% CI, 95% confidence interval.
To cite this abstract in AMA style:
McCormick N, Yokose C, Wei J, Lu N, Wexler D, De Vera M, Avina-Zubieta J, Zhang Y, Choi H. Comparative Effectiveness of Sodium-glucose cotransporter-2 Inhibitors for Recurrent Gout Flares and Gout-primary Emergency Department Visits and Hospitalizations: A General Population Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/comparative-effectiveness-of-sodium-glucose-cotransporter-2-inhibitors-for-recurrent-gout-flares-and-gout-primary-emergency-department-visits-and-hospitalizations-a-general-population-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparative-effectiveness-of-sodium-glucose-cotransporter-2-inhibitors-for-recurrent-gout-flares-and-gout-primary-emergency-department-visits-and-hospitalizations-a-general-population-cohort-study/