Session Information
Date: Saturday, November 6, 2021
Title: Epidemiology & Public Health Poster I: COVID-19 & Vaccination (0084–0117)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: While patients with systemic rheumatic diseases (SRDs) are in general more vulnerable to infections due to their underlying immune dysregulation and immunomodulatory therapies, data related to COVID-19 is conflicting. Early case series suggest that patients with SRD do not have more severe outcomes from COVID-19. This contrasts with data from retrospective cohort studies which suggest that patients with SRD have higher risk of mechanical ventilation or intensive care unit (ICU) admission than age- and sex- matched patients without SRD. Prior studies have been limited by sample size, lack of comparator groups, and/or appropriate statistical analysis. We used a large, multicenter cohort of patients hospitalized with COVID-19 in New York City during the first wave of the pandemic to determine whether patients with SRD hospitalized with COVID-19 were at increased risk of severe outcomes.
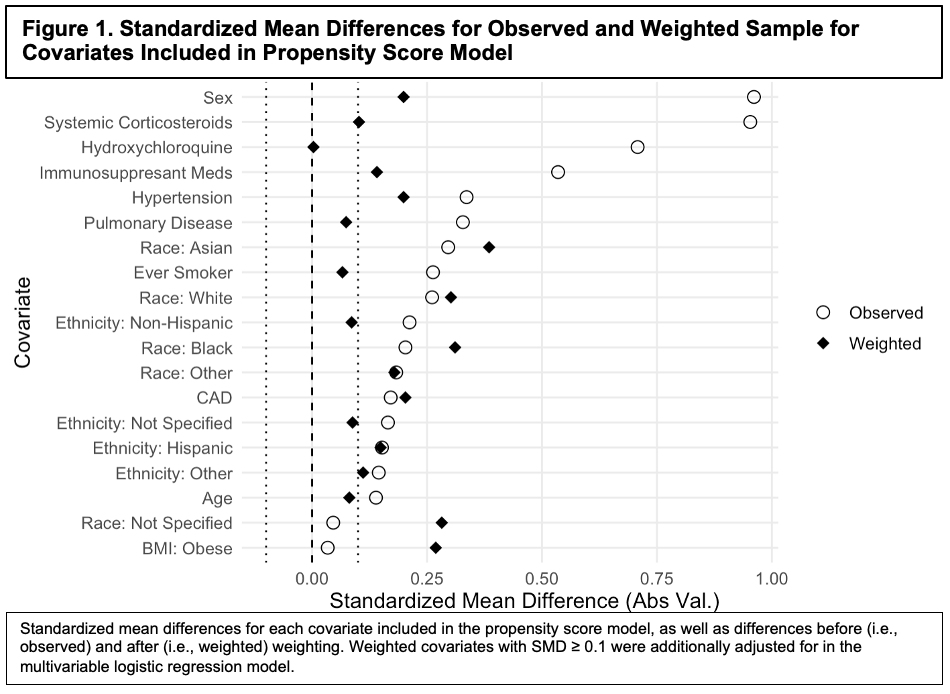
Methods: This retrospective observational cohort study included patients aged ≥18 years with confirmed SARS-CoV-2 infection hospitalized at any of three NewYork-Presbyterian hospital sites from March 3-May 15, 2020. We used chi-square tests and t-tests, as appropriate, to compare baseline characteristics, COVID-19-related symptoms, and outcomes between patients with and without SRD. Inverse probability of treatment weighting based on propensity scores (PS) was applied to a logistic regression model to assess the multivariable (MV) association between SRD status and the primary composite outcome of mechanical ventilation, admission to the ICU, or in-hospital death. Covariates with an absolute standardized mean (or proportion) difference (SMD) ≥0.10 in the PS model were adjusted for in the MV logistic regression outcome model (Figure 1).
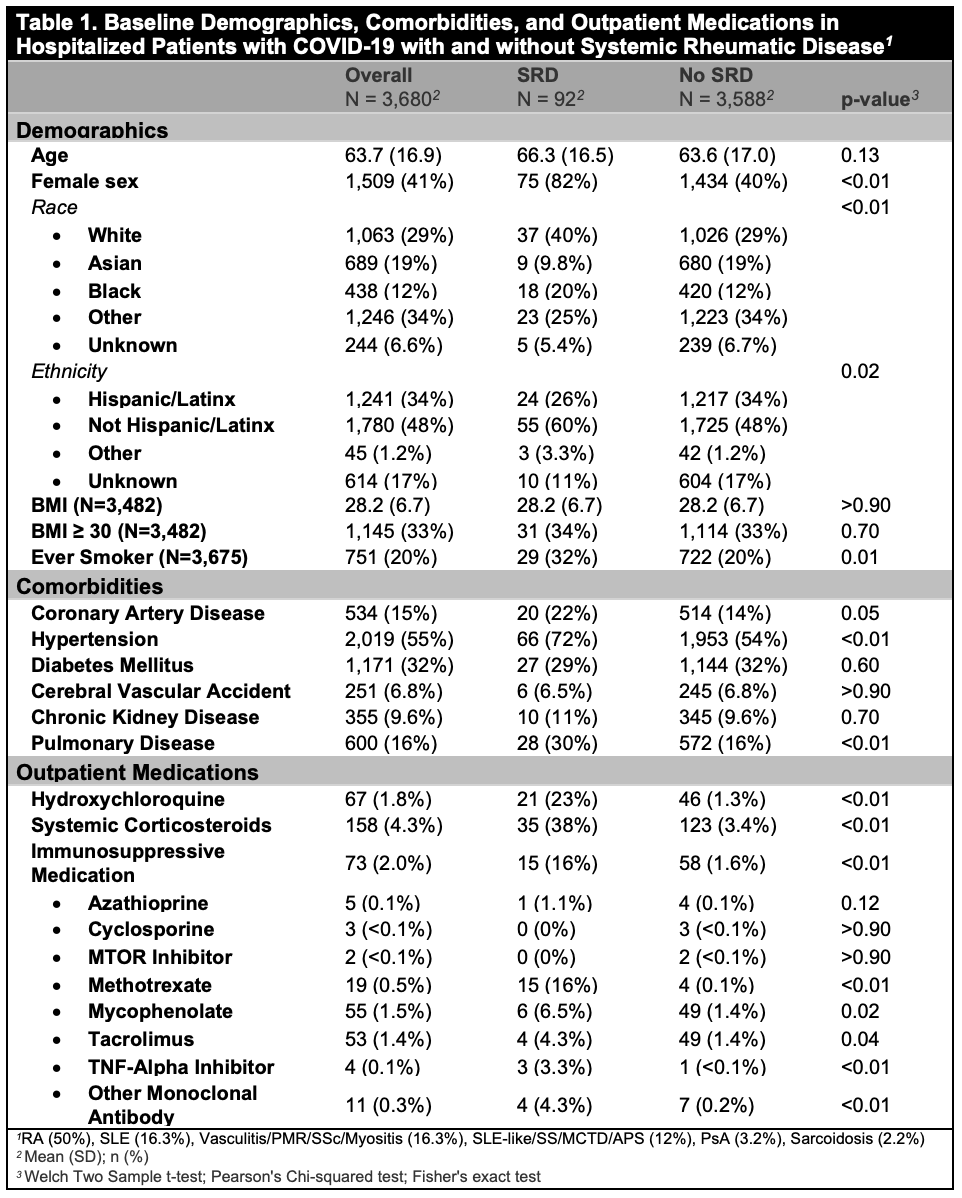
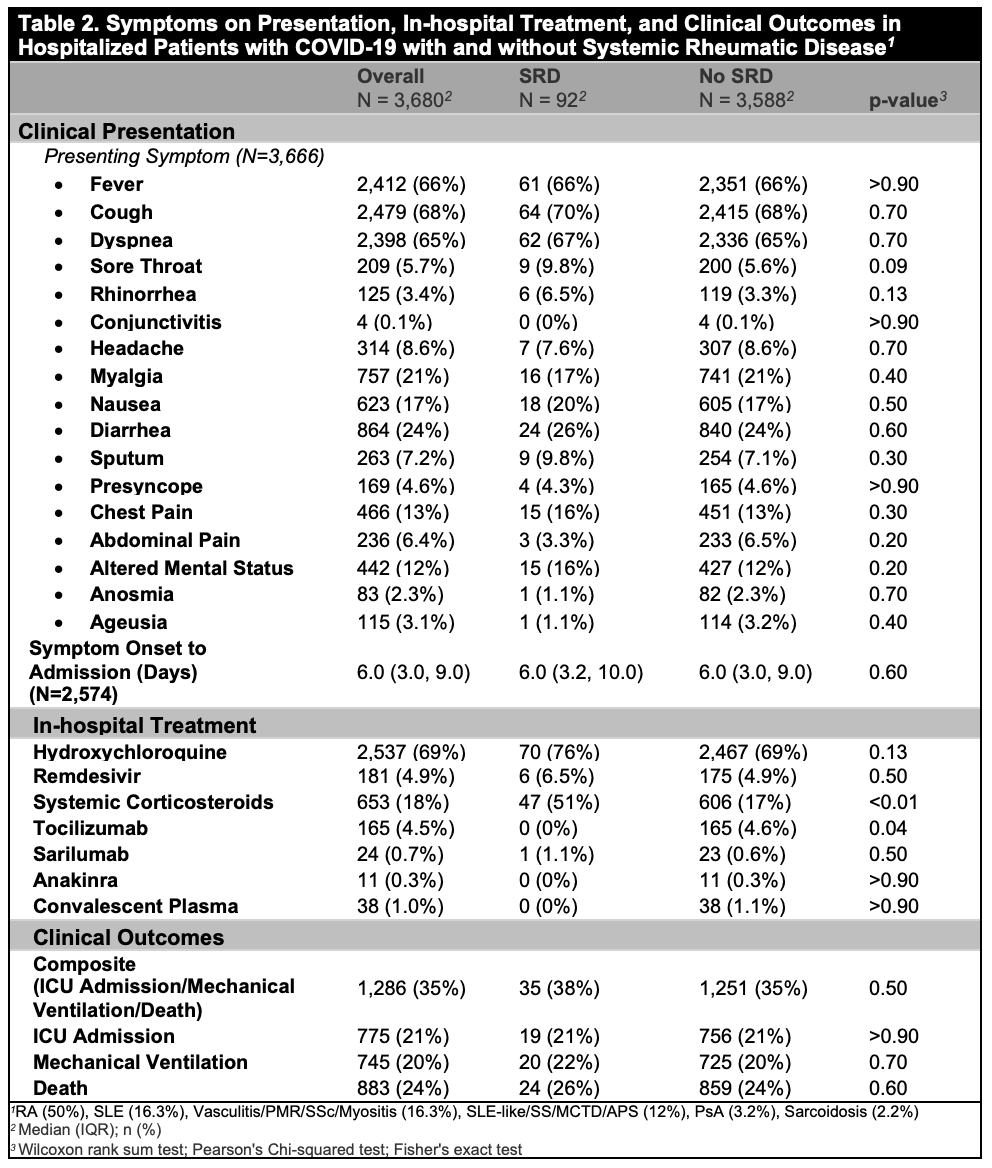
Results: Out of 3,680 patients hospitalized with COVID-19, 92 (2.5%) had SRD. Mean age of the cohort was 63.7 [16.9] years, and 41% were female, 29% White, and 34% Hispanic/Latinx. Compared to patients without SRD, patients with SRD had similar age and BMI, but were more likely to be female, ever smokers, White or Black, and less likely to be Hispanic/Latinx (Table 1). Patients with SRD had a higher proportion of coronary artery disease, hypertension, and pulmonary disease, as well as use of hydroxychloroquine, corticosteroids, and immunosuppressive medications than patients without SRD (Table 1). Although presenting symptoms were similar, patients with SRD were more likely than those without SRD to be treated with steroids during hospitalization (51% vs. 17%, p< 0.001) (Table 2). In the weighted MV analysis, patients with SRD had an OR of 1.27 [95% CI 1.12-1.44, p< 0.001] for the composite outcome of mechanical ventilation, ICU admission, or death compared to patients without SRD after adjustment for the remaining covariates with an absolute SMD ≥0.10.
Conclusion: During the initial peak of the pandemic in New York City, patients with SRD hospitalized with COVID-19 were 1.27 times more likely to experience mechanical ventilation, ICU admission, or death than patients without SRD. Our findings, which used inverse weighting to balance covariates in a large observational inpatient cohort in a COVID-19 “hotspot”, warrant confirmation in population-based cohorts.
To cite this abstract in AMA style:
Siegel C, Choi J, D'Angelo D, Christos P, Lally L, Goyal P, Mandl L, Barbhaiya M. Clinical Outcomes of Patients with Systemic Rheumatic Diseases Hospitalized for COVID-19 at a Large Academic Center in New York City [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/clinical-outcomes-of-patients-with-systemic-rheumatic-diseases-hospitalized-for-covid-19-at-a-large-academic-center-in-new-york-city/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-outcomes-of-patients-with-systemic-rheumatic-diseases-hospitalized-for-covid-19-at-a-large-academic-center-in-new-york-city/