Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: The clinical characteristics of dermatomyositis (DM) patients possessing the anti-Jo-1 autoantibody (autoAb) are not well known. We analyzed the clinical features and prognosis of Jo-1+ DM patients (Jo-1 DM) compared to Jo-1+ polymyositis (Jo-1 PM) patients.
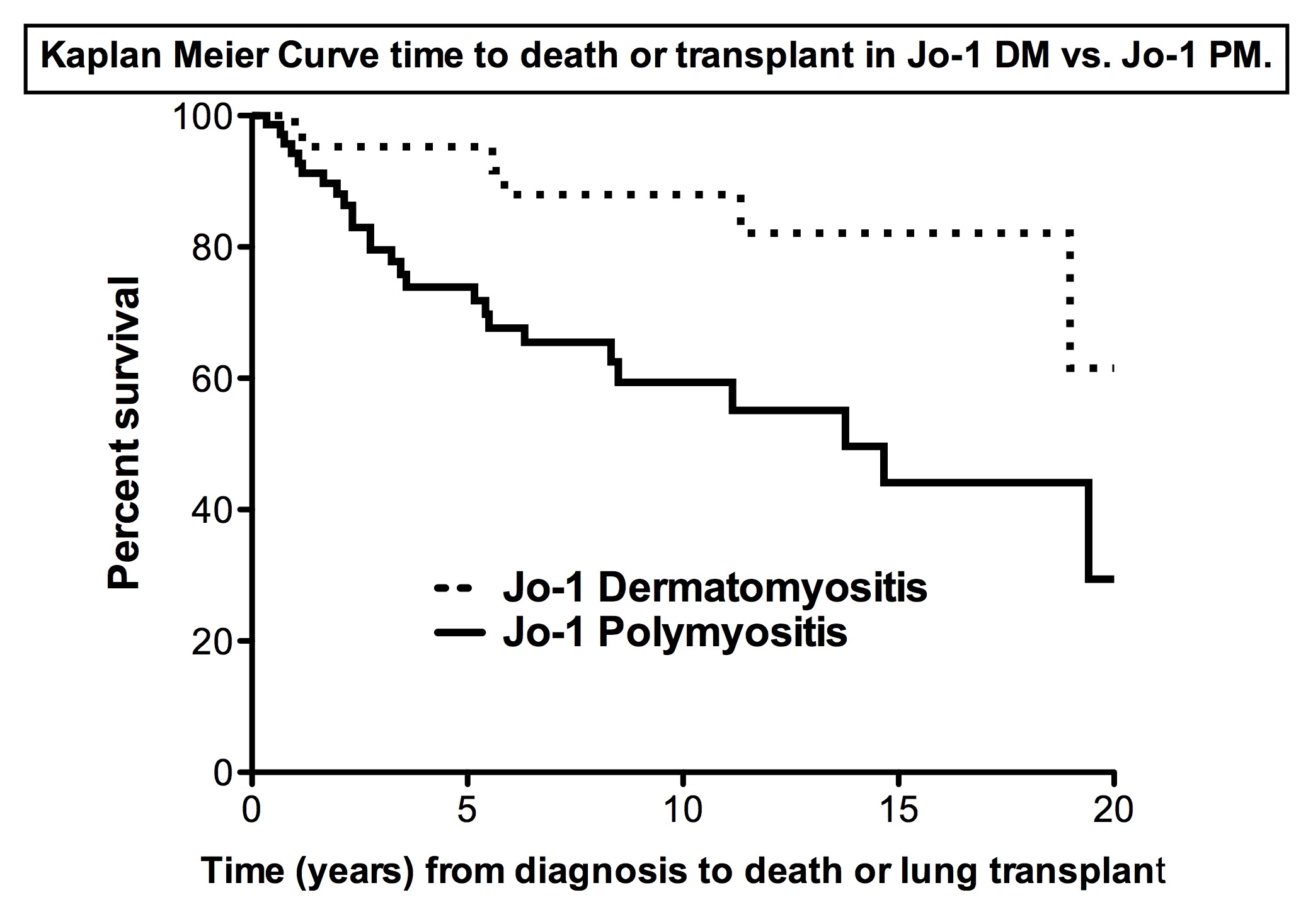
Methods: Jo-1+ patients were identified from a prospectively collected computer and serum database of adult myositis (n=856) patients seen from 1985 to 2012. Anti-Jo-1 was detected by immunoprecipitation and immunodiffusion in our research laboratory and probable or definite PM and DM were defined using Bohan and Peter criteria. Amyopathic and hypomyopathic DM was included in the DM cohort as per Sontheimer criteria. Designation of overlap syndrome and undifferentiated connective tissue disease (UCTD) was based on clinical diagnosis. Demographics, clinical and laboratory features were compared between Jo-1 DM and Jo-1 PM. Chi-square and t-tests were used for comparison. Survival (time to death) and pulmonary survival (death or transplant) was compared between the two groups from diagnosis using log rank test.
Results: 140 Jo-1+ patients in our cohort had available clinical data. 31% (44/140) were diagnosed as DM including 4 amyopathic DM and 11 hypomyopathic DM, 53% (74/140) had PM and 16% (22/140) had overlap or UCTD. There was no difference in gender (female 78% vs. 65%), age at diagnosis [mean (SD) years: 43.7 (12.8) vs. 47.1 (12.7)] or ethnicity (Caucasians: 87% vs. 88%) in Jo-1 DM vs. Jo-1 PM. All Jo-1 DM patients (except 3) had classic DM rashes including a heliotrope rash or Gottron papules or sign. Among DM rashes, Gottron papules, Gottron sign, heliotrope, other DM rashes (V-rash or shawl sign), periungual erythema, mechanics hands and periorbital edema were seen in 26%, 55%, 24%, 26%, 31%, 67% and 14%, respectively. There was no difference in Jo-1 DM vs. Jo-1 PM in the following CTD features: arthritis (46 %) vs. 44%), fever (31% vs. 52%), Raynaud (38% vs. 36%), dysphagia (21% vs. 19%), cardiac (4% vs. 3%) or primary pulmonary hypertension (5% vs. 3%). Mechanics hands were more common in Jo-1 DM as compared to Jo-1 PM (67% vs. 17%, p=0.001). Pulmonary involvement was very common and similar in both groups (89% vs. 95%) mostly due to pulmonary fibrosis (84% vs. 92%). Dyspnea (76% vs. 72%) or O2 supplementation (19% vs. 37%) was common in both groups as was muscle involvement (similar peak CK, proximal weakness and peak muscle disease activity (VAS) on the MDAAT). Significantly (p<0.01) fewer Jo-1 DM patients died [13.6% (6/44) vs. 33.3% (24/72)] as compared to Jo-1 PM. Cumulative survival and pulmonary survival (death or transplant) from diagnosis was significant better in patients with Jo-1 DM vs. Jo-1 PM (p< 0.004).
Conclusion: One-third of Jo-1+ patients have DM. Jo-1 DM and Jo-1 PM have similar clinical characteristics except for the rashes of DM and mechanic hands. DM Jo-1 patients had a better prognosis than Jo-1 PM.
Disclosure:
R. Aggarwal,
None;
D. Koontz,
None;
Z. Qi,
None;
C. V. Oddis,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-features-and-outcome-in-polymyositis-vs-dermatomyositis-patients-with-the-anti-jo-1-autoantibody/