Session Information
Date: Sunday, October 26, 2025
Title: (0357–0386) Patient Outcomes, Preferences, & Attitudes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: While UCTD is considered less clinically severe than SLE, our prior qualitative study reported that patients with UCTD experience significant psychosocial challenges (J Clin Rheumatol 2022). Here, we describe a large UCTD cohort and quantify psychosocial challenges in comparison to SLE.
Methods: This retrospective cohort study included patients aged ≥18 years enrolled in a UCTD or SLE academic hospital-based registry, January 2022-March 2025. Participants in the UCTD registry had a positive ANA, ≥1 sign/symptom of a CTD, and did not meet ACR/EULAR-endorsed classification criteria for SLE, RA, SSc, SS, Idiopathic Inflammatory Myopathy, or 2006 Revised Sapporo Criteria for APS. Participants in the SLE registry fulfilled 1997 ACR or 2019 ACR/EULAR SLE Classification Criteria. We administered the 36-Item Short Form Health Survey (SF-36) to assess health-related quality of life (HRQoL), Fatigue Severity Scale (FSS), General Anxiety Disorder-7 (GAD-7), and Beck Depression Inventory (BDI). We compared demographic and clinical variables and psychosocial questionnaire scores between patients with UCTD and SLE, and performed multivariable regression to evaluate the association between diagnosis and each psychosocial outcome, adjusting for demographic and treatment variables.
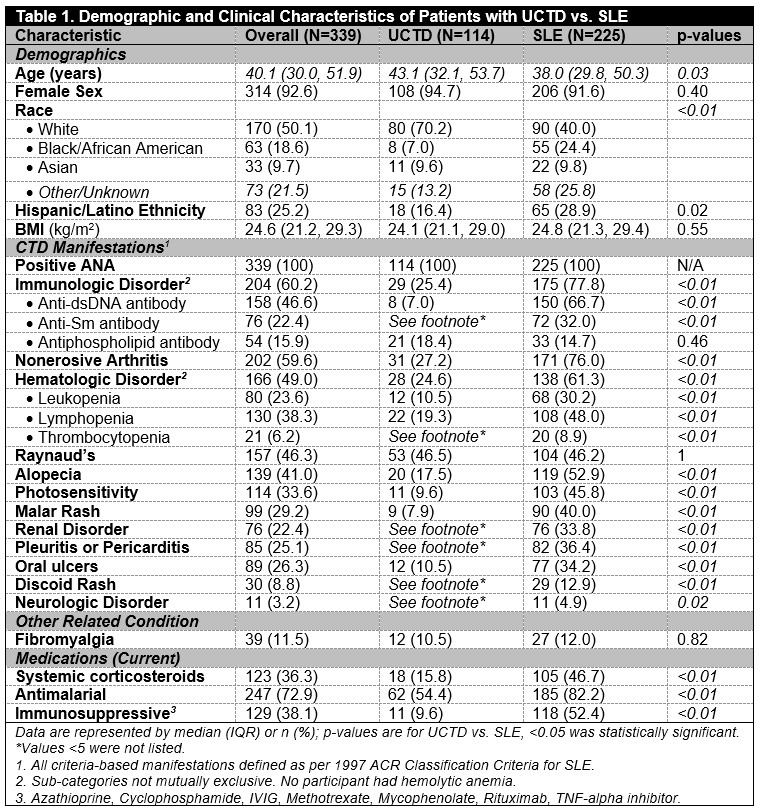
Results: Compared to individuals with SLE (Nf225), those with UCTD (n=114) were older (median [IQR] age 43.1 [32.1, 53.7] vs. 38.0 [29.8, 50.3], p=0.03), more frequently White race (70.2% vs. 40.0% p< 0.01), and less frequently Hispanic/Latino ethnicity (16.4% vs. 28.9%, p=0.02). Overall, patients with UCTD had fewer CTD manifestations. The most frequent clinical and serologic manifestations in UCTD, as compared to SLE, included: Raynaud’s (46.5% vs. 46.2%, p=1.00), arthritis (27.2% vs. 76.0%, p< 0.01), and lymphopenia (19.3% vs. 48.0%, p< 0.01). Patients with UCTD versus SLE were less frequently prescribed antimalarials (54.4% vs. 82.2%, p< 0.01) and immunosuppressive medications (9.6% vs. 52.4%, p< 0.01) [Table 1]. Compared to patients with SLE, those with UCTD had better SF-36-defined physical functioning (median [IQR] score 80.0 [60.0, 95.0] vs. 75.0 [50.0, 90.0], p< 0.05); other measures of HRQoL, fatigue, anxiety, and depression did not differ [Table 2].After multivariable adjustment, no association was demonstrated for diagnosis (UCTD vs. SLE) and HRQoL (based on SF-36 physical and mental component summary scores), FSS-defined fatigue severity, GAD-7-defined anxiety, or BDI-defined depression. In the overall group, female sex and non-Hispanic/Latino ethnicity were associated with worse SF-36 mental component summary scores. Female sex was associated with worse fatigue severity, and Hispanic/Latino ethnicity with increased odds of anxiety. Lastly, immunosuppressive treatment was associated with increased odds of depression [Table 3].
Conclusion: Patients with UCTD have fewer disease manifestations, less frequently require immunomodulatory/immunosuppressive treatment, and report better physical function than SLE comparators. Nonetheless, UCTD patients experience a similar degree of impaired HRQoL, fatigue, anxiety, and depression, suggesting they may benefit from dedicated psychosocial support.
To cite this abstract in AMA style:
Siegel C, Kim Y, Masto L, Nagpal N, Smole A, Sun D, Slosberg H, Minett M, Vega J, Jannat-Khah D, Salmon J, Lockshin M, Sammaritano L, Barbhaiya M. Clinical Characteristics and Psychosocial Outcomes of Patients with UCTD Compared to SLE [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clinical-characteristics-and-psychosocial-outcomes-of-patients-with-uctd-compared-to-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-and-psychosocial-outcomes-of-patients-with-uctd-compared-to-sle/

.jpg)
.jpg)