Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Early recognition and treatment of juvenile systemic lupus erythematosus (jSLE) improves outcomes and prevents disease-related mortality. This study examines the contributions of clinical factors (e.g. disease severity) and sociodemographic variables (e.g. neighborhood disadvantage, distance to care) to diagnostic delays.
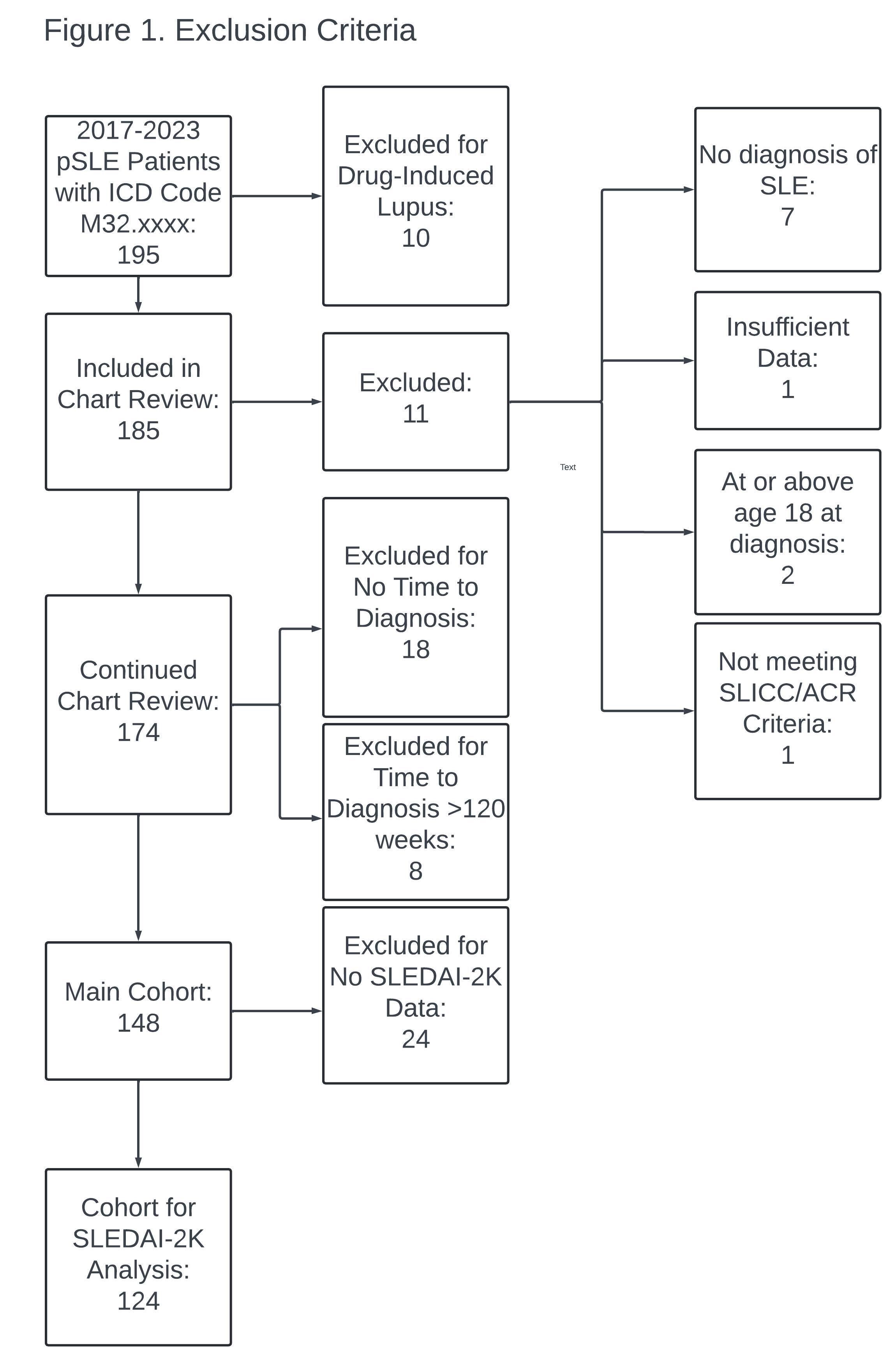
Methods: This retrospective chart review included jSLE patients evaluated by the Division of Pediatric Rheumatology at Indiana University (IU) from Jan 2017 – Sept 2023. Participants were diagnosed before age 18 years and fulfilled the 1997 American College of Rheumatology (ACR) or Systemic Lupus Collaborating Clinics (SLICC) criteria for SLE (Figure 1). Time to diagnosis (TTD) was treated categorically: acute ( 4 weeks), subacute (5-12 weeks), and chronic ( >12 weeks). Bivariate analyses were performed using Spearman correlation models and Wilcoxon-Kruskal-Wallis tests and multivariable analyses were performed using Generalized Linear Models, using SAS v9.4 (Figure 2).
Results: In bivariate analysis, the following clinical variables at diagnosis were associated with shorter TTD: neuropsychiatric symptoms (p=0.02), organ damage (p=0.04), pulse-dose corticosteroids (p=.01), and hospitalization (p=0.01). Higher disease activity at diagnosis, measured by SLEDAI-2K score, was associated with a trend towards shorter TTD when treated categorically, and this association reached significance when TTD was analyzed as a continuous variable (p= 0.04) (Figure 3). Renal disease was not associated with TTD. In bivariate analysis, private health insurance was associated with a longer TTD (p=0.04), while age, race, ethnicity, preferred language, urbanization level, distance to care, and ADI showed no association. In multivariable analysis including all variables with p < 0.10 plus age and sex, only the presence of neuropsychiatric symptoms remained independently associated with a shorter TTD (p = 0.02).
Conclusion: Neuropsychiatric symptoms, organ damage, pulse steroid use, and hospitalization at diagnosis were associated with shorter diagnostic intervals, suggesting that more severe presentations may prompt faster evaluation. Private health insurance was associated with a longer time to diagnosis, potentially reflecting differences in healthcare access or referral patterns. Race, ethnicity, distance to care, and area-level deprivation index were not significantly associated with diagnostic delays. The lack of association may reflect the single-center design, which could limit variability in access to care and sociodemographic representation. While several clinical variables were associated with a shorter TTD in the bivariate analysis, only neuropsychiatric symptoms remained significant in the multivariate analysis. The diminished effects of the other clinical variables suggest either mediating or confounding effects which will be explored in further analysis. The study findings underscore the complex interplay between disease severity and healthcare system factors in influencing diagnostic timelines for pediatric lupus.
.jpg) Figure 2. Bivariate and multivariable analysis of factors associated with Time to Diagnosis in juvenile Systemic Lupus Erythematosus (jSLE) (Nf148)
Figure 2. Bivariate and multivariable analysis of factors associated with Time to Diagnosis in juvenile Systemic Lupus Erythematosus (jSLE) (Nf148)
.jpg) Figure 3. Scatterplot of Time to Diagnosis vs Disease Activity at Diagnosis
Figure 3. Scatterplot of Time to Diagnosis vs Disease Activity at Diagnosis
To cite this abstract in AMA style:
Harter M, Hetrick R, Slaven J, Rodriguez M. Clinical and Sociodemographic Factors Associated with Diagnostic Delays in Pediatric Lupus Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clinical-and-sociodemographic-factors-associated-with-diagnostic-delays-in-pediatric-lupus-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-sociodemographic-factors-associated-with-diagnostic-delays-in-pediatric-lupus-patients/