Session Information
Date: Sunday, November 7, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Manifestations (0855–0896)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Lupus enteritis (LE) is a potentially life-threatening manifestation of systemic lupus erythematosus (SLE), with an incidence ranging from 8% to 27%. Timely diagnosis is essential for prompt treatment and the prevention of complications. As the clinical and immunological characteristics of LE have not been established in Latin American patients (1-2), we conducted a case-control study to investigate the clinical and serological characteristics compared with non-LE patients.
Methods: We performed a case-control study in SLE patients (per ACR criteria) at a tertiary care academic center from January 2012 to December 2019. Eleven patients with LE (cases) were matched with twenty-four non-LE patients (controls), who were similar in age and gender distribution to those of the group of cases. Descriptive statistics were used to compare them.
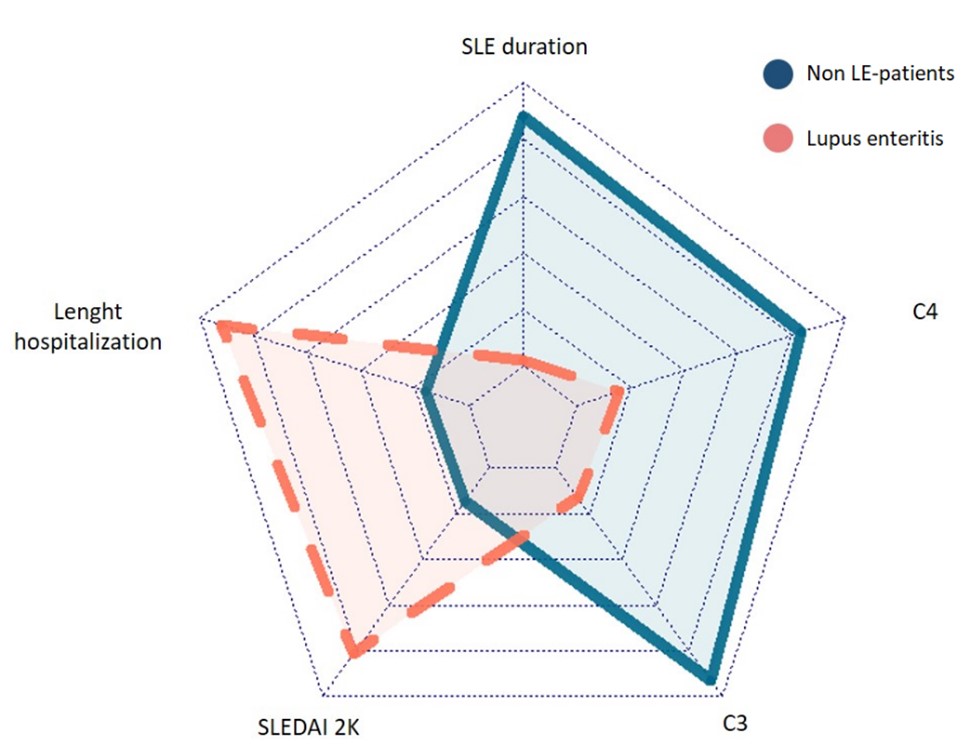
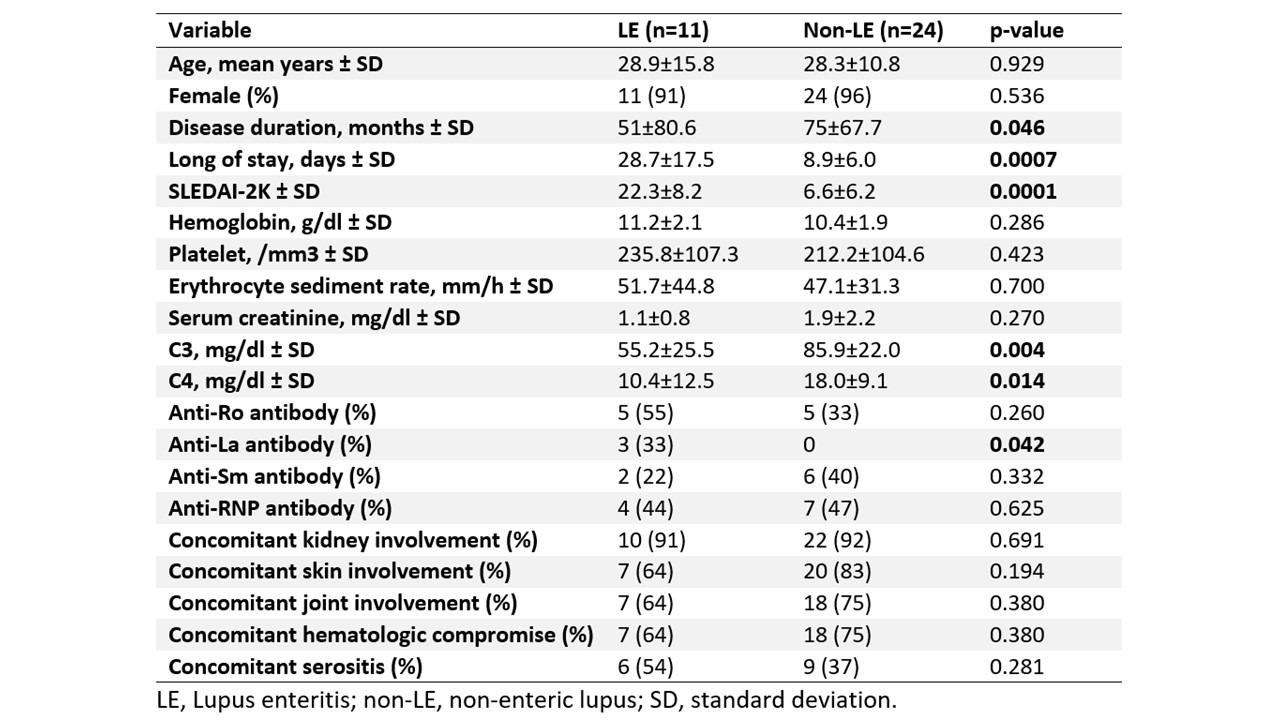
Results: LE patients were predominantly women (91%) and had a median age of 29 years. In seven (63.6%) patients LE was an initial presentation of SLE, 2 (18%) patients had a recurrence of LE, and 10 (90.9%) patients had concomitant lupus nephritis (LN). The most common clinical manifestations were abdominal pain (90.9%), nausea or vomiting (72.7%), fever (63.6%), and diarrhea (63.6%). Imaging studies revealed the target sign (63.6%), increased attenuation of mesenteric fat (18%), and bladder wall thickening (9.1%). Only one death was recorded and was due to sepsis. All patients received steroids as initial treatment, 82% intravenous (IV) pulses of methylprednisolone, 72.7% IV cyclophosphamide, 9.1% azathioprine, 9.1% mycophenolate mofetil, 9.1% rituximab, and 9.1% IV immunoglobulin. Among the eight patients who received cyclophosphamide, seven had LN or another severe SLE manifestation, which was the main indication for the additional immunosuppressant. LE patients had a significantly shorter disease duration (51 vs 75 months, p=0.046), longer hospital stay (28.7 vs 8.9 days, p=0.0007), higher SLEDAI-2K scores (22.3 vs 6.6, p=0.0001), lower levels of C3 (55.2 vs 85.9 mg/dL, p= 0.004) and C4 (10.4 vs 18.0 mg/dL, p= 0.014), and higher positivity of anti La antibodies (33.3% vs 0%, p= 0.042) compared to non-LE patients.
Conclusion: In Latin American patients, LE is an early SLE manifestation and often with coexistent LN. LE patients had evidence of more active disease than those without LE and had a moderate recurrence rate despite aggressive immunosuppressive therapy.
To cite this abstract in AMA style:
Muñoz-Urbano M, Sanchez-Bautista J, Santamaria-Alza Y, Quintero-González D, Ramirez A, Vanegas-García A, Vasquez G, Gonzalez L. Clinical and Serological Characteristics of Latin American Patients with Lupus Enteritis: A Case-Control Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/clinical-and-serological-characteristics-of-latin-american-patients-with-lupus-enteritis-a-case-control-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-serological-characteristics-of-latin-american-patients-with-lupus-enteritis-a-case-control-study/