Session Information
Date: Monday, November 18, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Polymyositis (PM), dermatomyositis (DM), and anti-synthetase syndrome (AS) are conditions included among idiopathic inflammatory myopathies (IMs).. Interstitial lung disease (ILD) is one of the most severe extra-muscular features.
To identify clinical risk factors associated with ILD in a well-defined monocentric cohort of 213 IM patients.
Methods: Data were prospectively collected between January 2005 and June 2023. Patients were regularly followed for a median of 72.6 months. Clinical data were collected in detail, including general data (ie, age, sex, and time since the first symptoms appeared), clinical manifestation. (type of organ involvement), data on histopathological findings (muscle biopsy), functional (electromyography, pulmonary function tests) and imaging (nailfold capillaroscopy-NC, HRCT). Laboratory data were collected at the same time, including a Hep-2 test, a test to detect antibodies against extractable nuclear antigens and a test to detect myositis-specific antibodies (D-Tek: BlueDiver Dot Myosits)
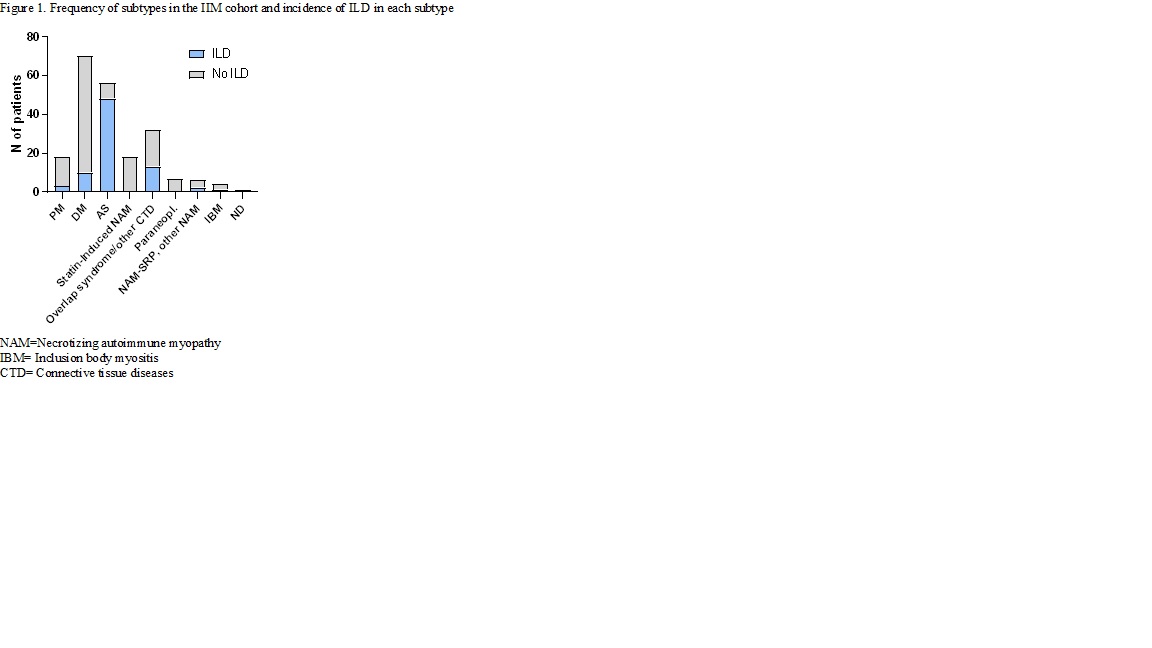
Results: The median patients age was 63 years (interquartile range 35.1-126.9), 69,7% were females. The frequency of IM subtypes in the cohort are presented in Figure 1. ILD was diagnosed in 77 patients. The most common pattern on HRCT was non-specific interstitial pneumonia (46%) followed by organizing pneumonia (20%). In ILD patients, dyspnoea and cough was the first sign of disease in 48.5% of patients, joint problems in 22.8%, muscle pain and weakness in 20.7%, and skin symptoms in 9.1%. ILD was significantly more frequent in AS (48/54; 88.8%) (p < 0.001), less frequently in PM (3/16; 18,7%) and in DM (9/67;13,4%), and none in statin myopathy. 19 patients with AS and ILD had the amyopathic form of IM. The AS subgroup was statistically significantly associated with the combination of anti-Ro 52 and anti-synthetase (most frequently Jo-1) AB (p< 0,01). There have been 12 ILD in 30 overlap syndromes, mostly overlaps with systemic sclerosis and the dominant AB was anti PM-Scl. We did not find a relationship between any antibody in PM, DM and ILD, but microvasculopathy detected by NC (non-specific abnormalities or systemic sclerosis pattern) was associated with DM-ILD and AS-ILD (p< 0,03). It was not related to the presence of the Raynaud‘s phenomenon, which was present only in 50% of patients with pathological NC.
Conclusion: Pulmonary symptoms may be the first sign of IM, therefore IM should be considered in all patients with ILD.
Anti-Ro 52 ABs, alone or in combination with anti-synthetase AB (mostly anti-Jo-1) are strongly suggestive of ILD. We observed an association between the pathological NC pattern and ILD, even in the absence of Raynaud‘s phenomenon.
To cite this abstract in AMA style:
Praprotnik S, Perdan-Pikmajer K, Lakota K, Rotar Z, Hocevar A. Clinical and Laboratory Features Associated with Pulmonary Involvement in Patients with Inflamatory Myopathy [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-and-laboratory-features-associated-with-pulmonary-involvement-in-patients-with-inflamatory-myopathy/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-laboratory-features-associated-with-pulmonary-involvement-in-patients-with-inflamatory-myopathy/