Session Information
Date: Friday, November 6, 2020
Session Type: Abstract Session
Session Time: 3:00PM-3:50PM
Background/Purpose: Relapsing polychondritis (RP) is a rare, heterogenous, systemic inflammatory disease with a predilection for cartilaginous structures. Recently we discovered myeloid-restricted somatic mutations in UBA1 in patients with a spectrum of adult-onset inflammatory diseases, and 60% of these patients were diagnosed with RP. Hematologic mosaicism for variants within a single residue of UBA1 now defines a novel syndrome called VEXAS (vacuoles, E1 enzyme, X-linked, autoinflammatory,somatic). The study objectives were to determine the prevalence of VEXAS in a cohort of patients with RP, to compare their clinical, laboratory, and immunologic features and to develop a clinical algorithm to inform genetic screening for VEXAS among patients with RP.
Methods: Patients that met diagnostic criteria for RP and were ≥18 years old were included. All patients were screened by whole-exome sequencing and UBA1 variants of interest were confirmed by Sanger sequencing. To determine prevalence of VEXAS within RP, UBA1 variants were tested in all patients enrolled in a large, prospective, observational cohort of RP. Additional patients with VEXAS were recruited from other cohorts and included in subsequent analyses. Immune populations were quantified by multipanel flow cytometry. Categorical and continuous variables were compared using the chi square or Kruskal-Wallis test. Random forest was used to create an algorithm to identify patients with VEXAS based on key clinical features. P< 0.05 defined statistical significance.
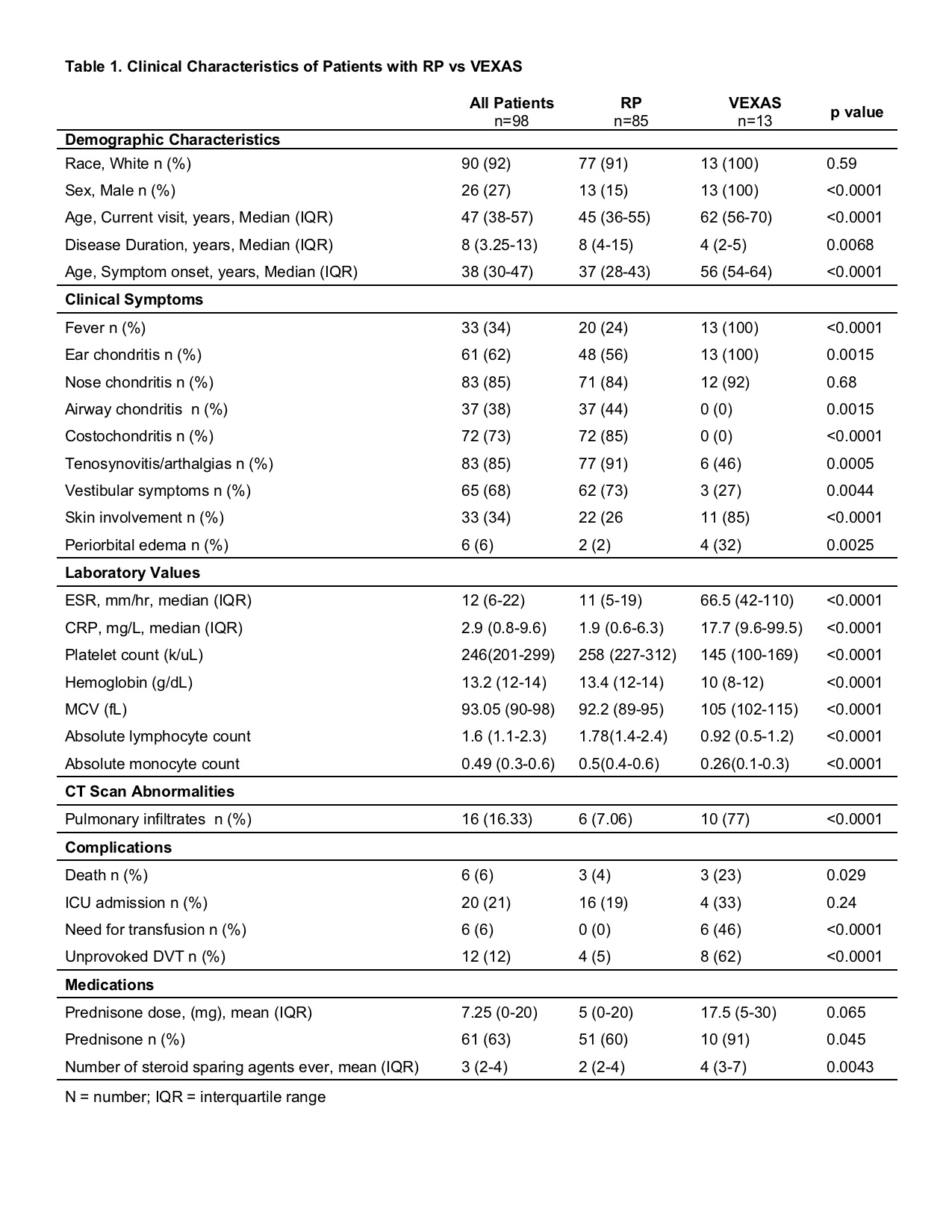
Results: Within a prospective cohort of 92 patients with RP, 7 patients were confirmed to have UBA1 variants consistent with VEXAS (prevalence=8%). Six additional patients with VEXAS from other cohorts were included for subsequent analyses. Compared to RP, patients with VEXAS were all male, older at disease onset, and more likely to have fever, ear chondritis, periorbital edema, skin involvement, deep vein thrombosis, and pulmonary infiltrates. Patients with RP as compared with VEXAS had a significantly higher prevalence of airway chondritis, costochondritis, tenosynovitis/arthralgias, and vestibular symptoms (Table). Mortality was significantly greater in VEXAS than RP (27% vs 2% p=0.01). Maximum ESR, CRP, and mean corpuscular volume (MCV) values were significantly greater in VEXAS. Absolute monocyte, lymphocyte, and platelet counts were significantly lower in VEXAS. Reduction of B lymphocytes and nonclassical monocytes (CD14-/CD16+) relative to healthy controls was observed in both RP and VEXAS, but was more marked in VEXAS. Increased Th17 cells was observed only in RP. A decision tree based on 1) Male sex or age at onset >50, 2) MCV >100 and 3) platelet count< 200 classified between VEXAS and RP with 100% sensitivity and 96% specificity.
Conclusion: Mutations in UBA1 are causal for disease in 8% of patients with RP. These patients have unique clinical characteristics that readily distinguish them from other patients with RP. A screening algorithm based on four, easily measurable clinical variables differentiates between VEXAS and RP with near-perfect accuracy. Early disease detection and improved clinical management is important in VEXAS given the high rate of mortality in this genetic subset of RP.
To cite this abstract in AMA style:
Ferrada M, Sikora K, Savic S, Luo Y, Wells K, Rose E, Quinn K, Goodspeed W, Jones A, Le M, Ombrello A, Deng Z, Gadina M, Tsai W, Aksentijevich I, Kastner D, Beck D, Grayson P. Classification of Patients with Relapsing Polychondritis Based on Somatic Mutations in UBA1 [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/classification-of-patients-with-relapsing-polychondritis-based-on-somatic-mutations-in-uba1/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/classification-of-patients-with-relapsing-polychondritis-based-on-somatic-mutations-in-uba1/