Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: To evaluate serum cytokine and chemokine profiles in patients with ANCA-associated vasculitis (AAV) classified by ANCA specificity (proteinase 3 (PR3)-ANCA versus myeloperoxidase (MPO)-ANCA) or by clinical diagnosis (granulomatosis with polyangiitis (GPA) versus microscopic polyangiitis (MPA)).
Methods: A panel of 29 soluble mediators involved in the pathogenesis of AAV was tested in active AAV patients at inclusion in a large randomized clinical trial. The levels of each biomarker were compared between groups within each classification system, ANCA type (PR3-AAV vs MPO-AAV) and clinical diagnosis (GPA vs MPA). Multivariable analyses corrected for age, sex, and renal insufficiency (eGFR<60ml/min/1.73m2) were also performed, with each biomarker as the dependent variable and ANCA type/clinical diagnosis as the explanatory variables of interest.
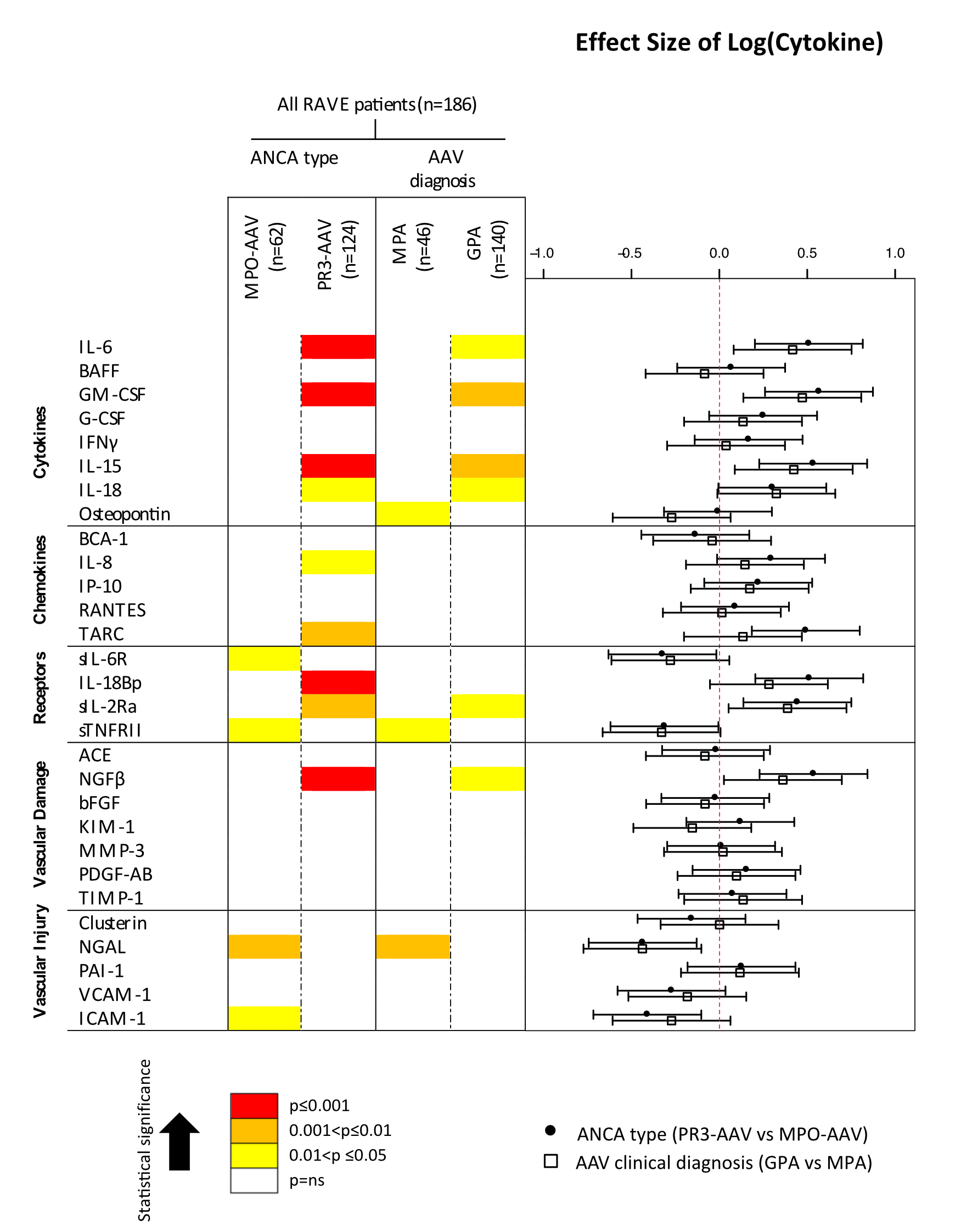
Results: The 186 subjects included 92 male and 94 female patients with median age 52 (IQR 44-66; range 15-92), all of whom had severe disease: median BVAS/WG 8 (IQR 5-10, range 3-23). Among these patients, 140 had been diagnosed with GPA and 46 with MPA; 124 were positive for anti-PR3 and 62 for anti-MPO. In each pair of groups (AAV clinical diagnosis, ANCA type) median BVAS/WG levels and number of patients on steroid or immune-suppressive treatment were not significantly different (p>0.05 in all comparisons). Levels of 9 mediators were significantly higher in PR3-AAV (IL-6, GM-CSF, IL-15, IL-18, IL-8, TARC, IL-18Bb, sIL-2Ra, NGFb; p<0.05), compared to 4 cytokines that were higher in MPO-AAV (sIL6R, sTNFR II, NGAL, ICAM-1; p<0.05). In contrast, only 6 cytokines (IL-6, GM-CSF, IL-15, IL-18, sIL-2Ra, NGFb; p<0.05) were higher in GPA than MPA, and 3 (Osteopontin, sTNFR II, NGAL; p<0.05) were higher in MPA than GPA. Although not formally compared, for nearly all biomarkers the difference between PR3-AAV/MPO-AAV was larger than that between GPA/MPA (Figure). The multivariate analysis showed that 8 soluble mediators (IL-15, IL-8, IL-18Bp, NGF-b, ICAM-1, TARC, Osteopontin, KIM-1; p<0.05) distinguished with more accuracy AAV patients when grouped for ANCA type rather than for clinical diagnosis.
Conclusion: According to serum biomarkers, ANCA specificity better discriminates distinct subsets of patients when compared to clinical diagnosis, suggesting important differences in underlying pathophysiology and justifying stratification of patients by ANCA specificity for treatment trials. Moreover, these findings suggest that expression of certain combination of cytokines and chemokines may be driven by and/or potentially impact pathways more active in PR3-AAV than in GPA, MPA and MPO-AAV, irrespective of severity of the disease.
Figure. Serum biomarkers’ association with ANCA type and AAV clinical diagnosis groups (PR3-AAV vs MPO-AAV and GPA vs MPA).
To cite this abstract in AMA style:
Berti A, Warner R, Johnson K, Cornec D, Schroder D, Kabat B, Merkel PA, Langford CA, Hoffman GS, Kallenberg CGM, Seo P, Spiera RF, St. Clair E, Stone JH, Specks U, Monach PA. Circulating Cytokine Profiles Reflect ANCA Specificity in Patients with ANCA-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/circulating-cytokine-profiles-reflect-anca-specificity-in-patients-with-anca-associated-vasculitis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/circulating-cytokine-profiles-reflect-anca-specificity-in-patients-with-anca-associated-vasculitis/