Session Information
Date: Monday, November 13, 2023
Title: (1082–1099) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid arthritis (RA) face an increased risk of herpes zoster (HZ) infection, notably those on immunosuppressive therapy. Herpes zoster infection is associated with comorbidities and a significant economic burden. The American College of Rheumatology recommends the recombinant herpes zoster vaccine for all immunocompromised adults above 18. We aimed to assess the current state of herpes zoster vaccination rates among RA patients at the Stanford Rheumatology Clinic and identify barriers to vaccination.
Methods: We retrospectively collected data from 1,449 consecutive RA patients seen at the Stanford Rheumatology Clinic from October 2017 to October 2022. We reviewed electronic medical records (EMR) to determine patients’ characteristics and HZ vaccination status. We categorized medication history based on ever being prescribed; 1) Janus Kinase inhibitor (JAKi), 2) biologic DMARDs (bDMARD), including anti-TNF, anti-IL6, anti-IL1, and anti-CD20, 3) conventional synthetic DMARDs (csDMARD) and 4) Hydroxychloroquine. We surveyed 19 current physicians (attendings and fellows) in the Rheumatology clinic to evaluate their practice patterns on vaccine discussions.
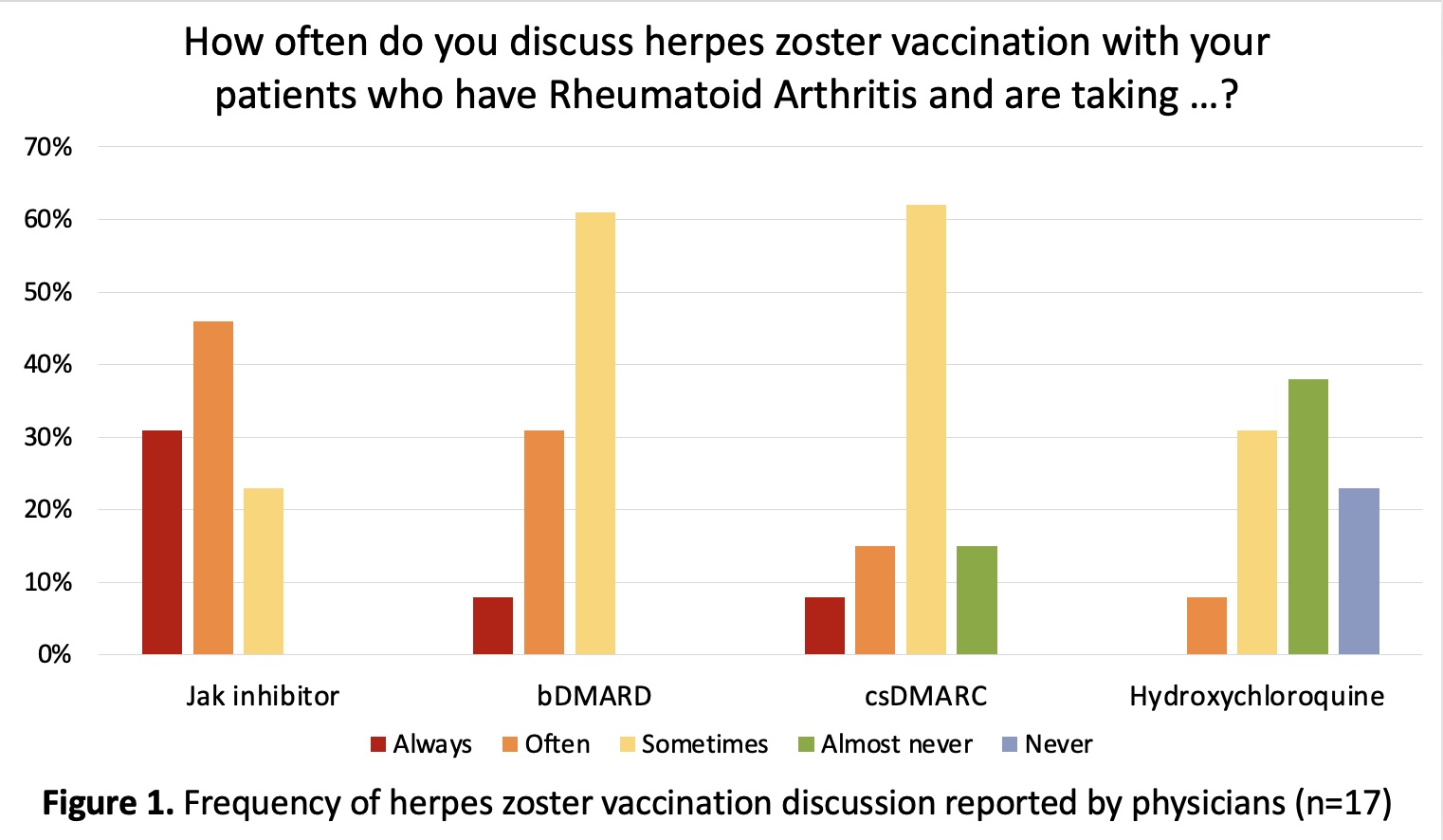
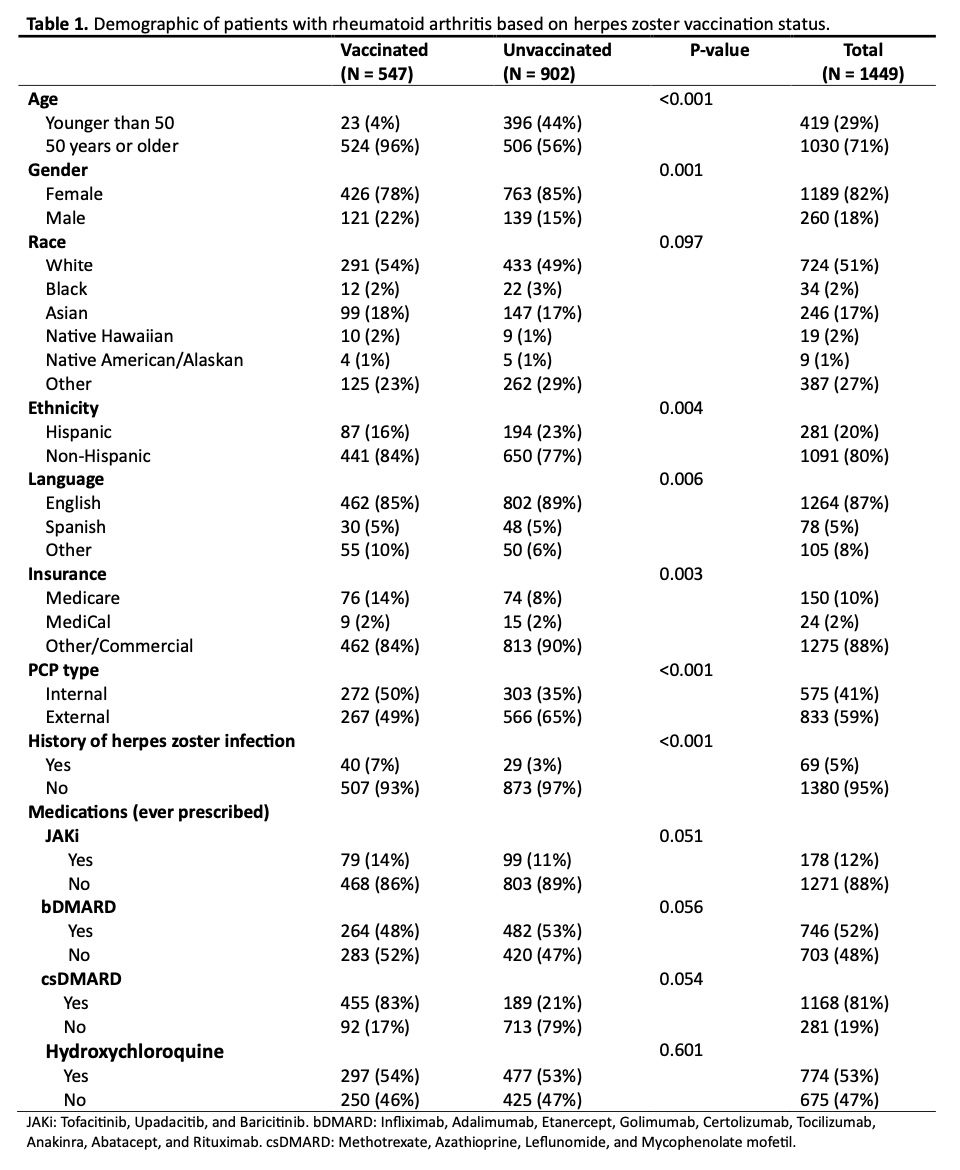
Results: Seventeen providers responded to the physician survey. We found that 61% “sometimes” discuss HZ vaccination with their RA patients, and 46% depend on primary care providers for vaccine discussions. Figure 1 shows the physician-reported HZ vaccination discussion rate based on the medication group. Our RA patient population were mostly female (82%) and 50 years old or older (71%). Among the 1,449 RA patients, only 547 (37.7%) have had HZ vaccination. Among those aged below 50 years, only 23 (5.5%) were vaccinated. Among the 178 patients who had ever been prescribed a JAKi, only 79 (44.4%) had the HZ vaccine, and most (90%) were aged 50 years or older (Table 1). The rate of Herpes Zoster vaccination was statistically different based on gender, ethnicity, primary language (English, Spanish, other), insurance type (Medicare, MediCal, Other/Commercial), PCP type (internal, external), and history of Herpes Zoster infection. We did not observe a statistically significant association between vaccination rate and specific immunosuppressive medication.
Conclusion: We identified a suboptimal herpes zoster vaccination rate among RA patients in our clinic, particularly those younger than 50 years on immunosuppressive therapy, including JAKi. We initiated an intervention to improve vaccine awareness by having the medical assistants inquire about the patient’s herpes zoster vaccine history during the clinic pre-calls. Patients were also encouraged to have further discussions with their rheumatologists. In addition to promoting patient education and physician awareness, potential future strategies to improve the vaccination rate include fostering collaboration with primary care providers, engaging with pharmacies on campus to make the HZ vaccine readily accessible, and developing automatic reminders in the electronic medical system. Additional efforts, e.g., overcoming insurance barriers, may be needed for at-risk patients younger than 50.
To cite this abstract in AMA style:
Faghihi-Kashani S, Babar A, Lin J. Characterizing Herpes Zoster Vaccination Patterns in Rheumatoid Arthritis Patients in a Tertiary Care Clinic: A Quality Improvement Approach [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/characterizing-herpes-zoster-vaccination-patterns-in-rheumatoid-arthritis-patients-in-a-tertiary-care-clinic-a-quality-improvement-approach/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterizing-herpes-zoster-vaccination-patterns-in-rheumatoid-arthritis-patients-in-a-tertiary-care-clinic-a-quality-improvement-approach/