Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Tissue-resident memory T cells (TRM) cells can drive localized, recurrent inflammation. TRM are site-specific T cells that take up long-term residence in peripheral tissues and aid in pathogen defense. Thus, the TRM in autoimmune disease is critical in respect to induction, chronicity, remission and relapse. Cellular/molecular biology of TRM in respect to their growth/cytokine net work in autoimmune disease is a new field and remains largely unknown. Here we have investigated the regulatory role of TRM in PsA; and have studied Rheumatoid arthritis (RA, as a positive control) and osteoarthritis (OA, as a negative control).
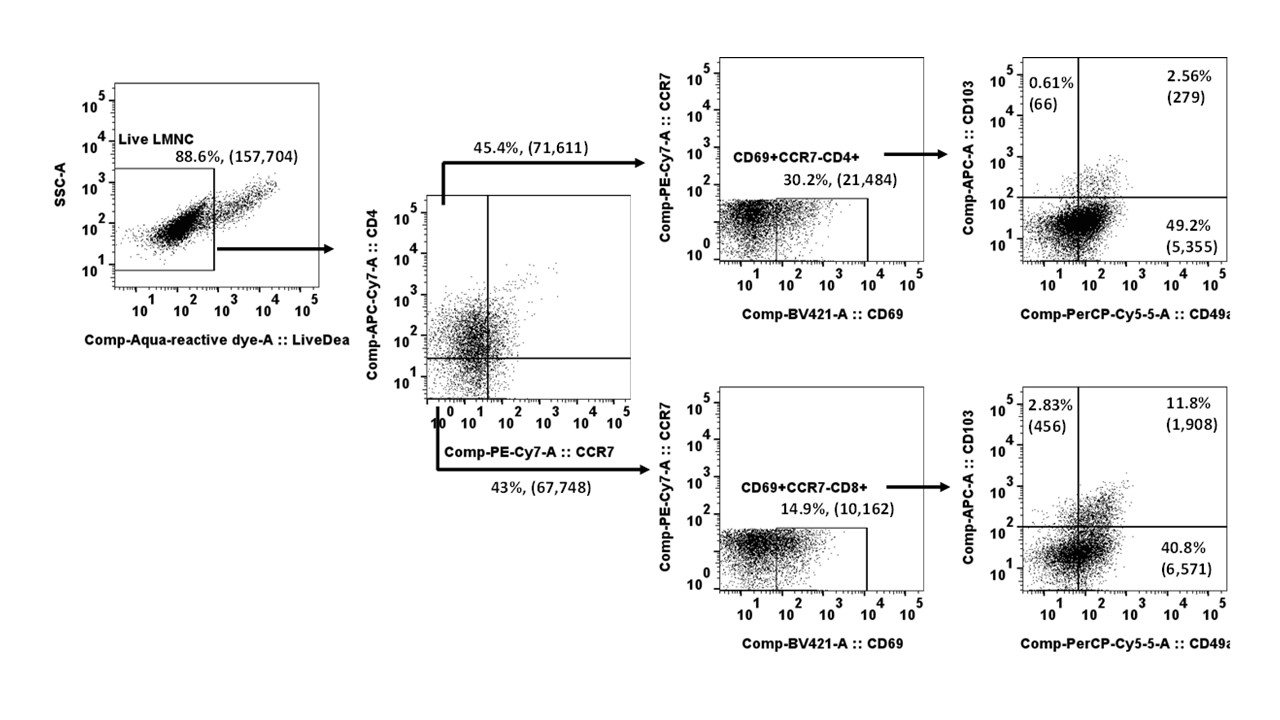
Methods: Synovial fluid mononuclear cells (SFMC) were collected from untreated/active age/sex matched, patients with PsA, RA, OA (n=12/each). SFMC cells (106 cells/mL) were activated with antihuman CD3/CD28 antibody cocktail; cells were cultured for 3 days. Hi-D FACS studies were done (i) to identify TRM (CCR7–CD69+CD103+/CD49a+) T cells (CD3+CD4+/CD8+) and (ii) to evaluate relevant Th1/Th17 cytokines (TNFα, IFNγ,IL-17A, IL-22) in TRM. MFI and the percentages of each cell population were analysed using a Flow Jo software. Results are described as Mean±SEM.
Results:
Here we phenotyped CD8+/CD4+ TRM cells (CCR7–CD69+CD103+ /CD49a+) in PsA and RA, and have noticed that they were of heterogeneous population characterized by multiple distinct phenotypes and functions (Figure 1).
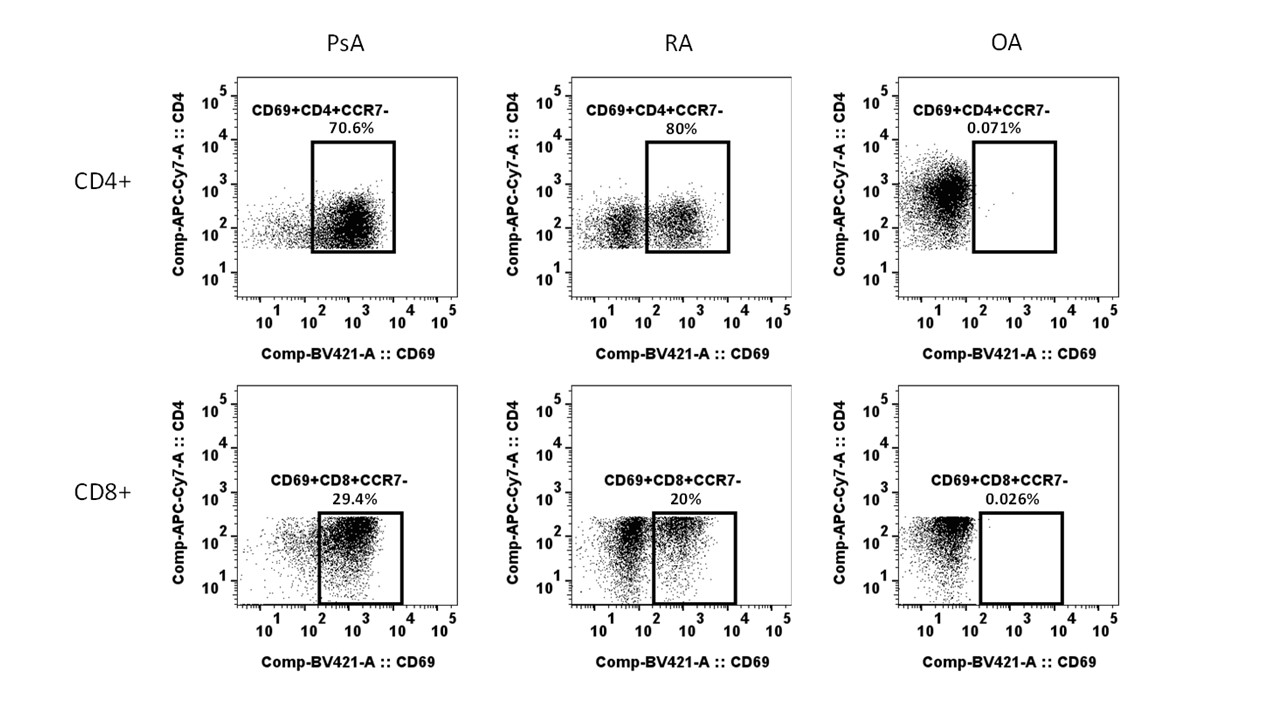
In live gated SFMC in PsA and RA the CD4+TRM cells were 20.5%± 3.5% and 18.5%±4.4% respectively compared to < 1% in OA (p< 0.001).
Majority of the CD3+ SFMC TRM cells in both PsA and RA were CD4+ ( >70%) (Figure 2). Thus the major source of the TRM cell derived Th1/Th17 cytokines were the CD4+TRM cells.
In PsA CD4+TRM cells; IL-17A (50.5%±1.5%), IL-17F (20.5%±2.5%) and IL-22 (25.5 %±1.3%) secreting cells were significantly higher (p< 0.01) than RA IL-17A (20.5%±1.4%) (IL-17F 10.9%±1.2%), IL-22 (15.5%±0.5%) ); whereas RA CD4+TRM cells had higher numbers of TNFα(24.3%±0.2%) and IFNγ producing cells(30.8%±0.5%); TNFα and IFNγ CD4+TRM cells in PsA were respectively 16±0.11% and 14.5% (p< 0.01).
Conclusion: Here we identified the synovial TRM cells in autoimmune arthritis in PsA and RA. This is the first study to substantiate the regulatory role of TRM cells in PsA. TRM cells are capable of site-specific flare after remission. Thus, our observations provide a novel insight that depletion of TRM cells as a potential long term remission for PsA. Further we noticed that TRM cells are skewed more towards the Th17 cells compared with RA; which indicates the impact of IL-23 on TRM cell growth/apoptosis and its therapeutic relevance in PsA.
To cite this abstract in AMA style:
Raychaudhuri S, Abria C, Raychaudhuri S. Characterization of the Tissue Resident Memorial T Cells in Autoimmune Arthritis: A Comparative Study of Psoriatic Arthritis and Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characterization-of-the-tissue-resident-memorial-t-cells-in-autoimmune-arthritis-a-comparative-study-of-psoriatic-arthritis-and-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-of-the-tissue-resident-memorial-t-cells-in-autoimmune-arthritis-a-comparative-study-of-psoriatic-arthritis-and-rheumatoid-arthritis/