Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Racial disparities in access to care and treatment regimens exist but remain poorly characterized in the rheumatoid arthritis (RA) patient population. Previous studies using the Ethnic Minority RA Consortium (EMRAC) have demonstrated non-Caucasian RA patients have a lower frequency of biologic use versus Caucasian patients despite controlling for comparable disease activity and access to treatment. Here we explore longitudinal racial disparities in rheumatoid arthritis treatment and emergency department (ED) use in a single tertiary academic center.
Methods: Structured de-identified data from 2010-2018 of patients who had at least two diagnoses of RA from a rheumatology outpatient encounter and at least one DMARD script during the follow-up period were extracted from the electronic health record of a single tertiary care center. Follow-up was measured from each patient’s first visit to each patient’s last visit within the 2010-2018 timeframe. Patient demographics were measured at the baseline visit, with medication use and comorbidities measured at baseline or at any point during follow-up. The average number of outpatient visits and ED visits per year (limited to ED visits within the health system) during follow-up were also measured. Differences in patient characteristics and visits were compared in patients who were black versus white based on standard t-test and χ2 analysis.
Results: A total of 1831 patients with rheumatoid arthritis were identified from 2010-2018. Baseline demographics were measured at each patient’s first visit and include mean [SD] age, 55.05 [14.47] years; 1499 [81.87%] female; and 991 [54.12%] white. Average [SD] duration of follow-up for all patients was 6.97 [2.28] years. Comparing black (n=639) and white (n=991) patient demographics, significant findings include that black patients were more likely to be older, have higher BMI, former or current smoking status, and have higher rates of diabetes and cardiovascular disease (p< 0.0001). Prednisone and csDMARD use were significantly more frequent in black patients compared to white patients (79.3% vs 69.1% p< 0.0001; 96.7% vs 93.5%, p=0.005, respectively). Biologic use was significantly more common among white patients compared to black patients (white 74.3%, black 67.0% p=0.001). In terms of site of care delivery, black patients had significantly more ED visits, with a median 0.24 ED visits per patient per year versus 0.00 for white patients. A summary of the findings are shown in Table 1.
Conclusion: Patients who were black were less likely to receive a biologic and more likely to use glucocorticoids. ED visit use was higher in black patients, which could be related to higher rates of comorbidities, although differences in geographic location could also influence whether patients visited an ED or saw non-rheumatology providers within or outside the health system. Further studies identifying drivers of racial disparities in access to care and outcomes are needed.
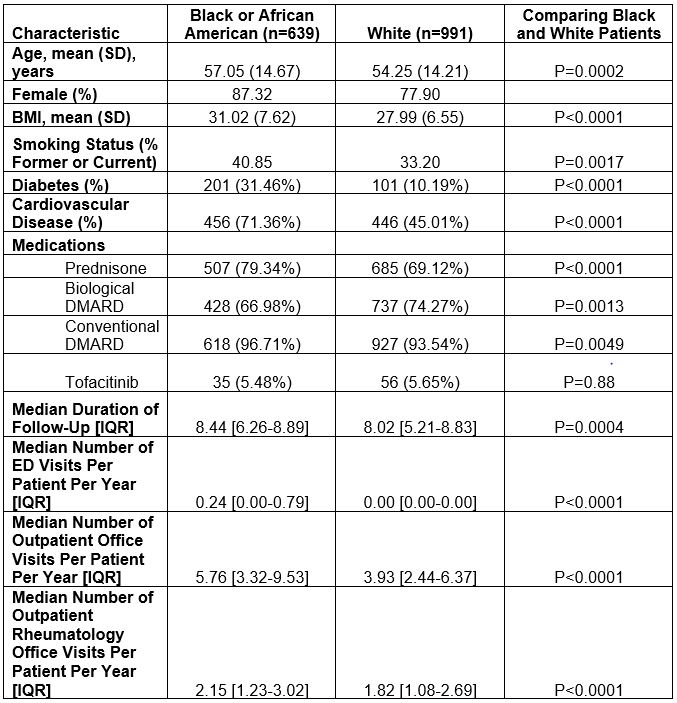 Comparison of Patient Characteristics
Comparison of Patient Characteristics
To cite this abstract in AMA style:
He E, Cornblath E, Yalamanchi P, Ogdie A, Baker J, George M. Characterization of Racial Disparities in Rheumatoid Arthritis Treatment Choice and Location of Care [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/characterization-of-racial-disparities-in-rheumatoid-arthritis-treatment-choice-and-location-of-care/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-of-racial-disparities-in-rheumatoid-arthritis-treatment-choice-and-location-of-care/
