Session Information
Date: Saturday, November 12, 2022
Title: Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Various pulmonary manifestations may occur in patients with antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV). ANCA-related interstitial lung disease (ILD) has recently been described in patients with or without overt AAV. The significance and evolution of this association remains unclear and has been raising research efforts in the past years. This study aims to compare 1) characteristics, 2) clinical course and 3) treatments of patients with ILD and positive ANCA, to those without positive ANCA.
Methods: A retrospective chart review was performed in all patients who had a follow-up from 2018 to 2021 at the ILD clinic or vasculitis clinic in our academic center. Patients with available ANCA results and at least two clinic visits were included. For each visit, data was collected regarding patient characteristics, clinical presentation, bloodwork, imaging, pulmonary function tests, hospitalizations, and treatments. Radiological patterns described on high resolution computed tomography (HRCT) stemmed from official reports generated by pulmonary radiologists and were validated by respirologists in charge of the ILD clinic. Descriptive statistics are reported to compare characteristics of patients with ANCA-related ILD, to those with ILD without positive ANCA.
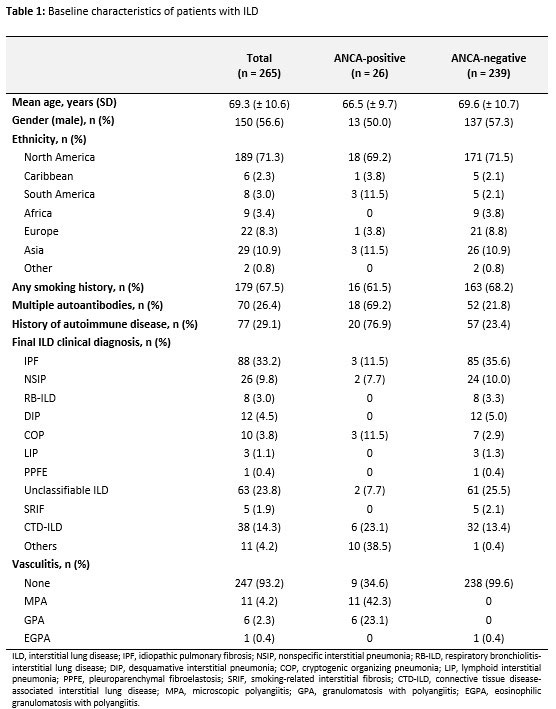
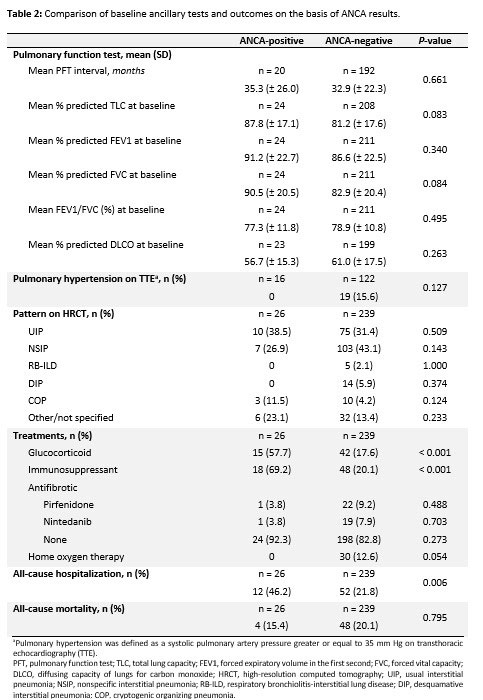
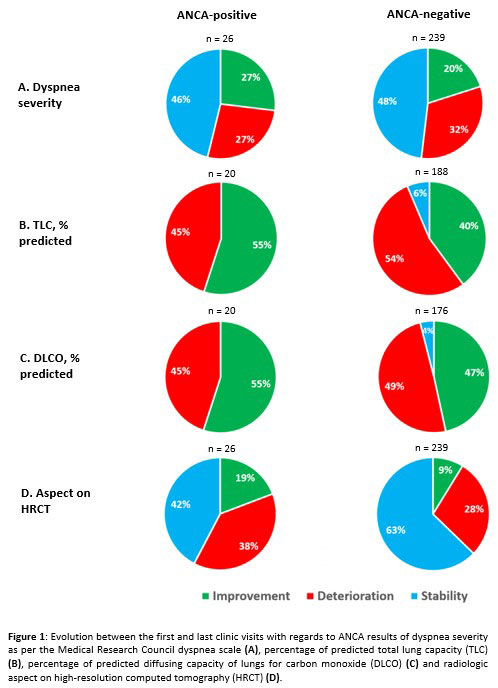
Results: 265 patients with ILD were included with a mean follow-up duration of 69.3 (± 10.6) months. Amongst these patients, 26 (9.8%) showed ANCA positivity (proteinase 3 and/or myeloperoxidase). Baseline characteristics are presented in table 1. The most frequent final clinical diagnosis in the ANCA-negative group was idiopathic pulmonary fibrosis, whereas connective tissue disease-associated ILD was more prevalent in the ANCA-positive group. The most common patterns on HRCT found in those with positive ANCA were usual interstitial pneumonia, nonspecific interstitial pneumonia and organizing pneumonia (table 2). A total of 17 (65.4%) patients with positive ANCA had a clinical diagnosis of AAV at some point during the follow-up period. In 5 (29.4%) patients, AAV developed following ILD diagnosis. No significant differences in pulmonary disease evolution over time was found between patients with ANCA-positive ILD and ANCA-negative ILD (figure 1). However, patients with ILD and positive ANCA received significantly more glucocorticoids, immunosuppressive therapy and had more hospitalizations of all cause (table 2).
Conclusion: This study involved a large cohort of patients with ILD. Due to the ANCA positivity rate and risk of developing AAV over time, ANCA testing should be considered in patients with ILD. Further prospective research is required to improve management of patients with ANCA-related ILD.
To cite this abstract in AMA style:
Bui K, Richard R, Drouin A, Toban N, Levesque M, Meunier R, Ross C, Makhzoum J. Characterization of Interstitial Lung Disease in the Presence of Antineutrophil Cytoplasmic Antibodies [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/characterization-of-interstitial-lung-disease-in-the-presence-of-antineutrophil-cytoplasmic-antibodies/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-of-interstitial-lung-disease-in-the-presence-of-antineutrophil-cytoplasmic-antibodies/