Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Antisynthetase syndrome (ASSD) is characterized by interstitial lung disease (ILD), myositis, polyarthritis, Raynaud’s phenomenon, dermatomyositis-like rash and mechanic’s hands. ILD may present with isolated antisynthetase-specific autoantibodies (AS-aAbs) without other ASSD features. The objective was to compare the characteristics and evolution of patients with ILD and AS-aAb with and without systemic manifestations of ASSD.
Methods: Patients evaluated at the ILD Clinic with AS-aAb detected by line blot assay (Euroimmun) were included. Patients were classified as ASSD if they had at least 1 other systemic manifestation(s) of ASSD, and otherwise as interstitial pneumonia with autoimmune features (IPAF) and non-IPAF according to 2015 ERS/ATS criteria. ILD progression was defined as meeting ATS/ERS/JRS/ALAT or OMERACT criteria, need for oxygen supplementation or lung transplant, or death. Time to ILD progression was analyzed using Kaplan-Meier and multivariable Cox analyses.
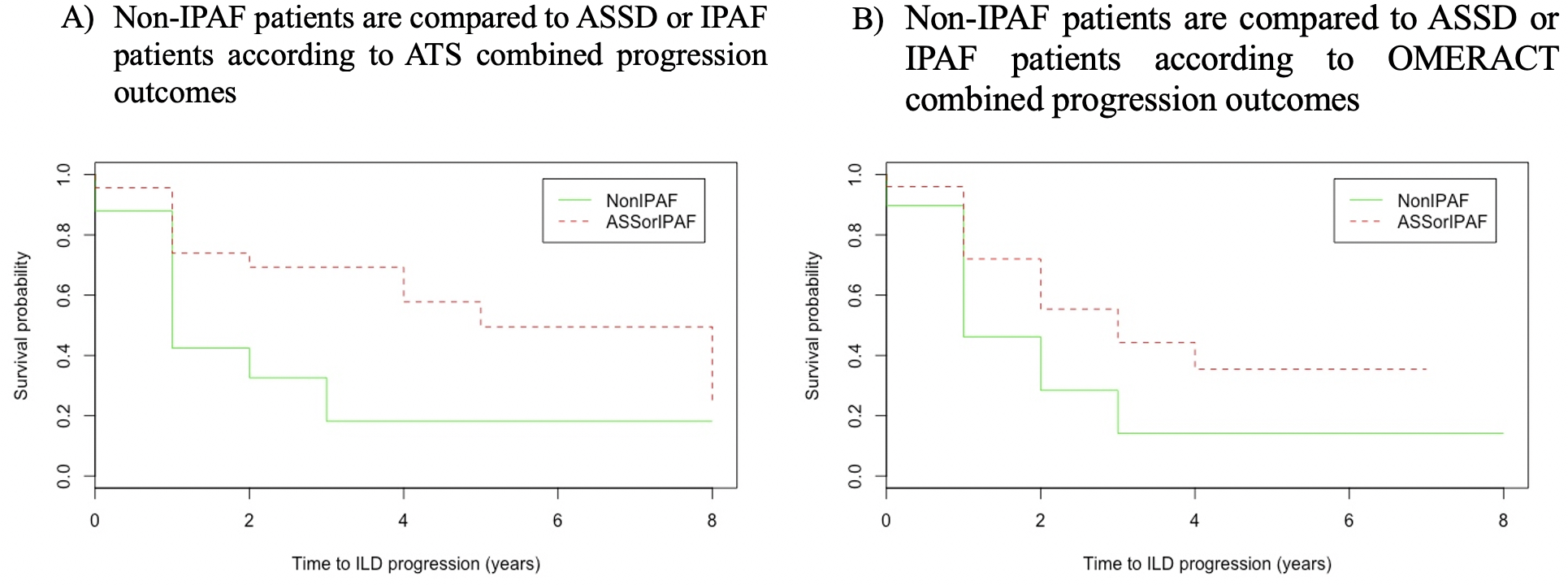
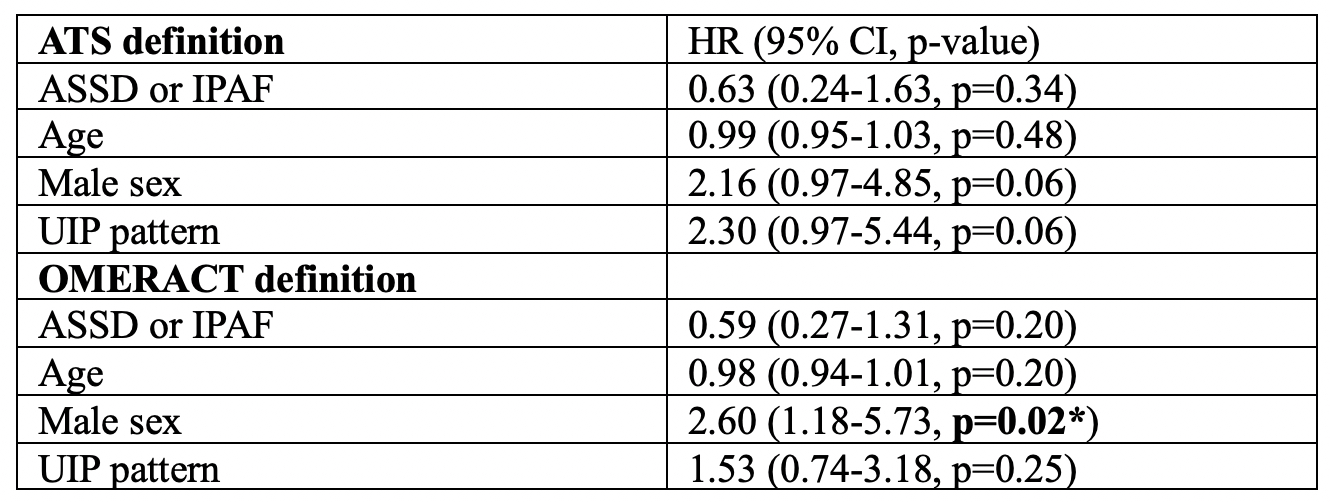
Results: Sixty-eight patients were included (12 ASSD, 13 IPAF, 43 non-IPAF). Most common AS-aAbs were anti-PL7/12 (71%). Mean age was 67 years, 69% were male, 87% were Caucasian and median follow-up was 2.4 [0.5,4.9] years. ASSD patients more frequently had concomitant anti-Ro52-aAbs (40% vs 5%, p=0.0004) and moderate-strong titers of AS-aAbs (60% vs 23%, p=0.004). Non-IPAF patients more frequently presented with usual interstitial pneumonia (UIP) pattern (64% vs 16%, p=0.0005) and were numerically more often male (74% vs 60%) with a smoking history (88% vs 68%) and moderate-severe ILD (56% vs 29%) on high-resolution CT scan. Antifibrotics were mainly used in non-IPAF patients (43% vs 4%, p=0.0006). Upon follow-up, 31 of 55 (56%) and 36 of 64 (56%) patients experienced ILD progression using ATS and OMERACT criteria, respectively. Unadjusted Kaplan-Meier analyses showed a protective association between ASSD/IPAF and ILD progression (HR 0.38, 95% CI: 0.19-0.78, p=0.008 using ATS; HR 0.47, 95% CI: 0.24-0.91, p=0.03 using OMERACT, see Figure). Multivariable Cox analyses showed that male sex was an independent predictor of ILD progression, and that non-IPAF and UIP pattern were numerically associated with increased risk (see Table). After multidisciplinary assessment, non-IPAF patients were ultimately diagnosed with idiopathic interstitial pneumonia (IPF) in 56%, non-classifiable in 30%, hypersensitivity pneumonitis in 10%, sarcoidosis in 2% and smoking-related ILD in 2% of cases.
Conclusion: In this AS-aAb-positive population, ILD progression was more frequent in men with UIP pattern irrespective of ASSD, IPAF and non-IPAF classification. Most non-ASSD patients in our cohort did not fulfill IPAF criteria and were ultimately diagnosed as IPF. Further study is required to identify predictors of progression while accounting for treatment effect and confounding by indication. Future classification criteria for ASSD should consider the reliability of AS-aAb detection using different methods.
*Drs Landon-Cardinal and Hoa contributed equally to this abstract.
To cite this abstract in AMA style:
Mourot A, Panuta B, Charbonneau J, Mounkam Ngeuleu A, Vo C, Rich E, Bourré-Tessier J, Villeneuve E, Manganas H, Gauthier A, Morisset J, Anh-Tu Hoa S, Landon-Cardinal O. Characteristics of Interstitial Lung Disease Progressors in an Antisynthetase Autoantibody-Positive Population [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characteristics-of-interstitial-lung-disease-progressors-in-an-antisynthetase-autoantibody-positive-population/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-interstitial-lung-disease-progressors-in-an-antisynthetase-autoantibody-positive-population/