Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with SLE have high rates of hospitalizations annually and require careful coordination of care in both the inpatient and outpatient setting. Prior analyses have shown how SLE patients from disadvantaged socioeconomic backgrounds are more likely to have multiple hospital admissions in comparison to their counterparts.1 In our own hospital system in Austin, Texas, almost half of our patients are uninsured or underinsured. The purpose of this project was to review the characteristics of hospital admissions of SLE patients in our hospital system and follow these patients’ transitions of care by reviewing outpatient rheumatology records.
-
Yazdany, J., Marafino, B. J., Dean, M. L., Bardach, N. S., Duseja, R., Ward, M. M., & Dudley, R. A. (2014). Thirty-day hospital readmissions in systemic lupus erythematosus: predictors and hospital- and state-level variation. Arthritis & Rheumatology, 66(10), 2828–2836. doi:10.1002/art.38768
Methods: Using Vizient database, we retrospectively reviewed patients hospitalized at Dell Seton Medical Center in Austin, Texas from 2020 – 2022 with an ICD-10 diagnosis code of SLE. We collected demographic data, information about the hospitalization and any subsequent admissions. For patients who were recommended rheumatology follow-up on discharge paperwork, we reviewed the chart records of our three outpatient rheumatology clinic sites to determine if patients attended their follow-up appointments.
Results: There were 125 admissions with an ICD diagnosis of SLE. 18 of these patients do not have a proven SLE diagnosis and were excluded.
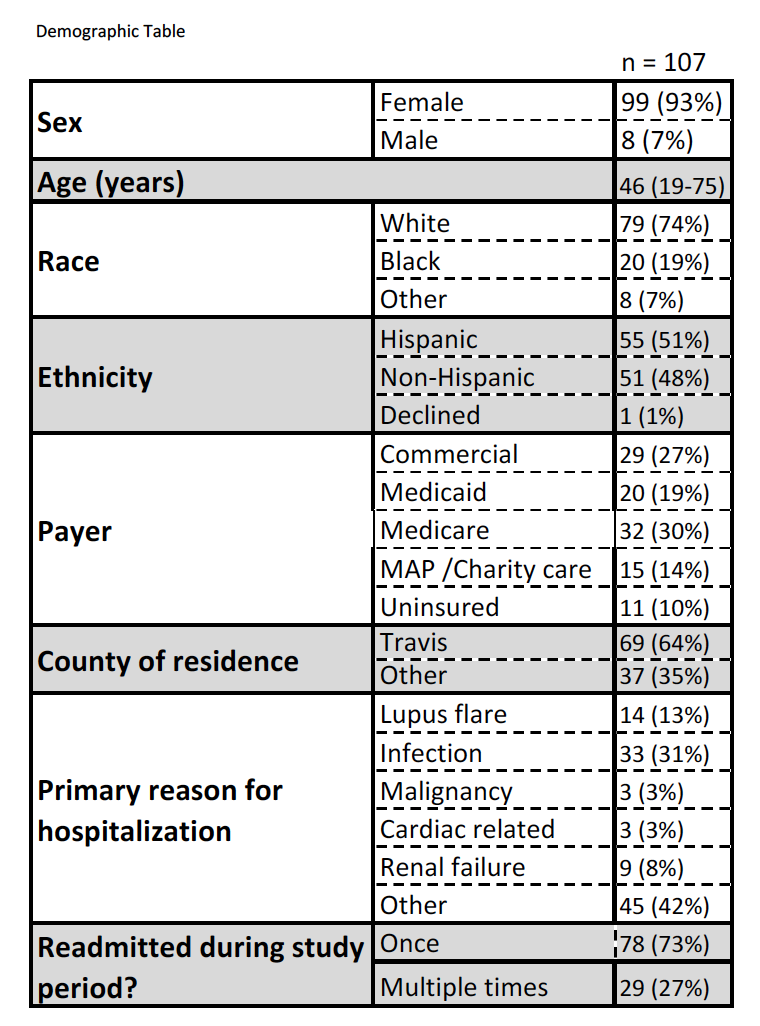
Of the 107 identified patients, majority were female (99/92%), White (79/74%), Hispanic (55/51%) and had commercial insurance (29/27%) (table 1). The most common admission reason was infection (33/31%). Our rheumatology team evaluated 33 of the 107 patients during their first admission (31%). 29 (27%) patients were readmitted during our study period (figure 1).
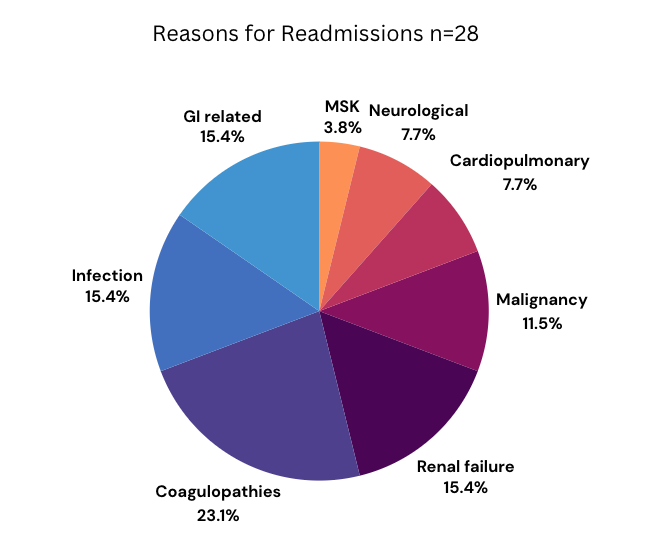
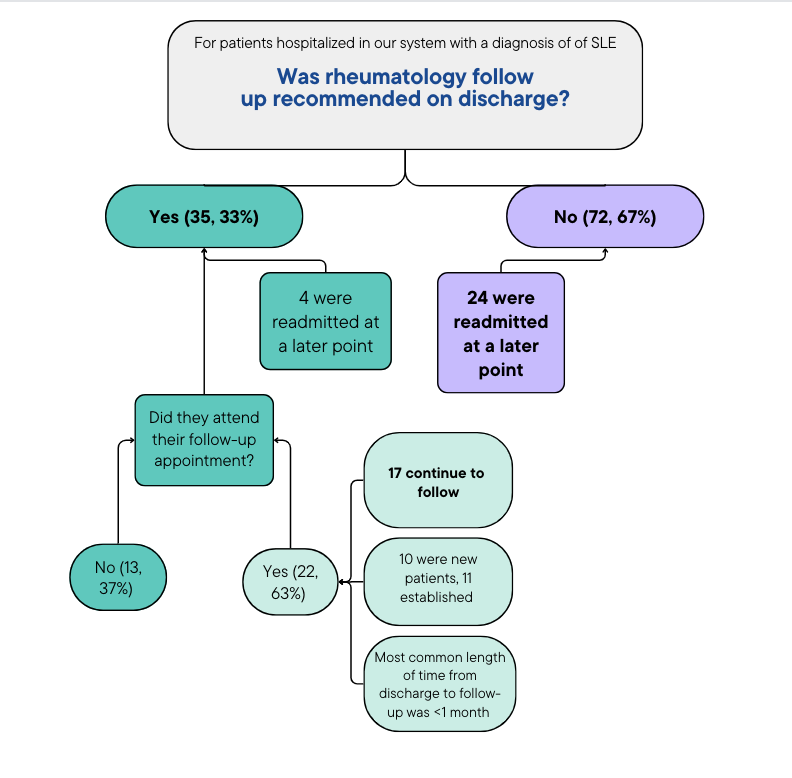
Rheumatology follow-up was recommended for 35 patients (33%) on discharge. Of these 35 patients, 22 made their post-hospital rheumatology appointment, and only 4 were readmitted at a later time in our study period. There were 72 patients (67%) who were not recommended follow-up on discharge. 24 of these patients were readmitted later in the study period. 77% of patients who made their initial post-hospitalization follow-up continued to follow at the clinic (figure 2).
Conclusion: This study provides insight into the care of SLE patients in our hospital system. It is reassuring that most patients who were recommended follow-up attended their appointment and continued to follow with an outpatient rheumatologist. Although SLE patients require complex coordination of care and need to see a rheumatologist on a regular basis, less than half of patients were recommended follow-up on discharge. Furthermore, those who were not recommended rheumatology follow-up were more likely to be readmitted compared to those who were. Now that this has been identified, our next step will be improve provider awareness of the importance of rheumatology follow-up in order to decrease readmission rates, and improve transitions of care for SLE patients with disadvantaged socioeconomic backgrounds.
To cite this abstract in AMA style:
Kotamarti R, Patel V. Characteristics of Hospitalizations and Outpatient Follow-up for Patients with SLE at an Academic Hospital Setting in Austin, Texas [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characteristics-of-hospitalizations-and-outpatient-follow-up-for-patients-with-sle-at-an-academic-hospital-setting-in-austin-texas/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-hospitalizations-and-outpatient-follow-up-for-patients-with-sle-at-an-academic-hospital-setting-in-austin-texas/