Session Information
Date: Saturday, November 6, 2021
Title: Epidemiology & Public Health Poster I: COVID-19 & Vaccination (0084–0117)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with systemic rheumatic diseases (SRD) are potentially at increased risk of severe outcomes from SARS-CoV-2 infection due to their underlying immune dysregulation and chronic use of immunosuppressive therapies. Older age, medical comorbidities, and steroid use have been identified as potential risk factors for COVID-19-related hospitalization in SRD patients, but still need to be confirmed. Our study aims to identify characteristics associated with severe COVID-19, characterized by mechanical ventilation, admission to an intensive care unit (ICU), or death, in patients with SRD hospitalized for COVID-19 in a U.S. “hotspot” during the initial wave of the pandemic.
Methods: This retrospective observational cohort study included patients aged ≥18 years with SRD hospitalized for COVID-19 at one of three NewYork-Presbyterian (NYP) hospital sites between March 3-May 15, 2020. Data were manually abstracted from the medical chart. We used chi-square tests and t-tests, as appropriate, to compare baseline demographics, comorbidities, outpatient medications, presenting symptoms, COVID-19 treatment, and laboratory values in patients hospitalized for COVID-19 with underlying SRD, stratified on the composite outcome of mechanical ventilation, ICU admission, or in-hospital death. We also examined the prevalence of secondary clinical outcomes in SRD patients.
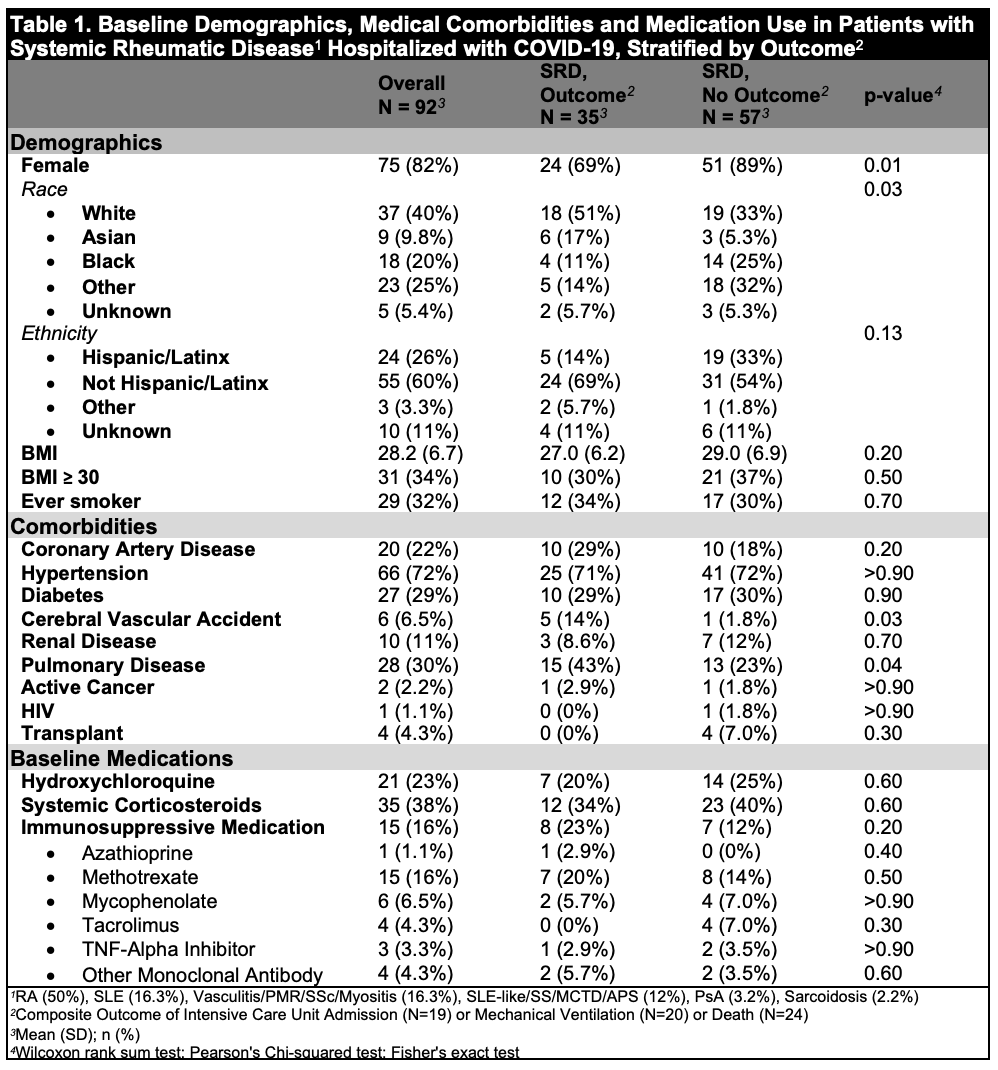
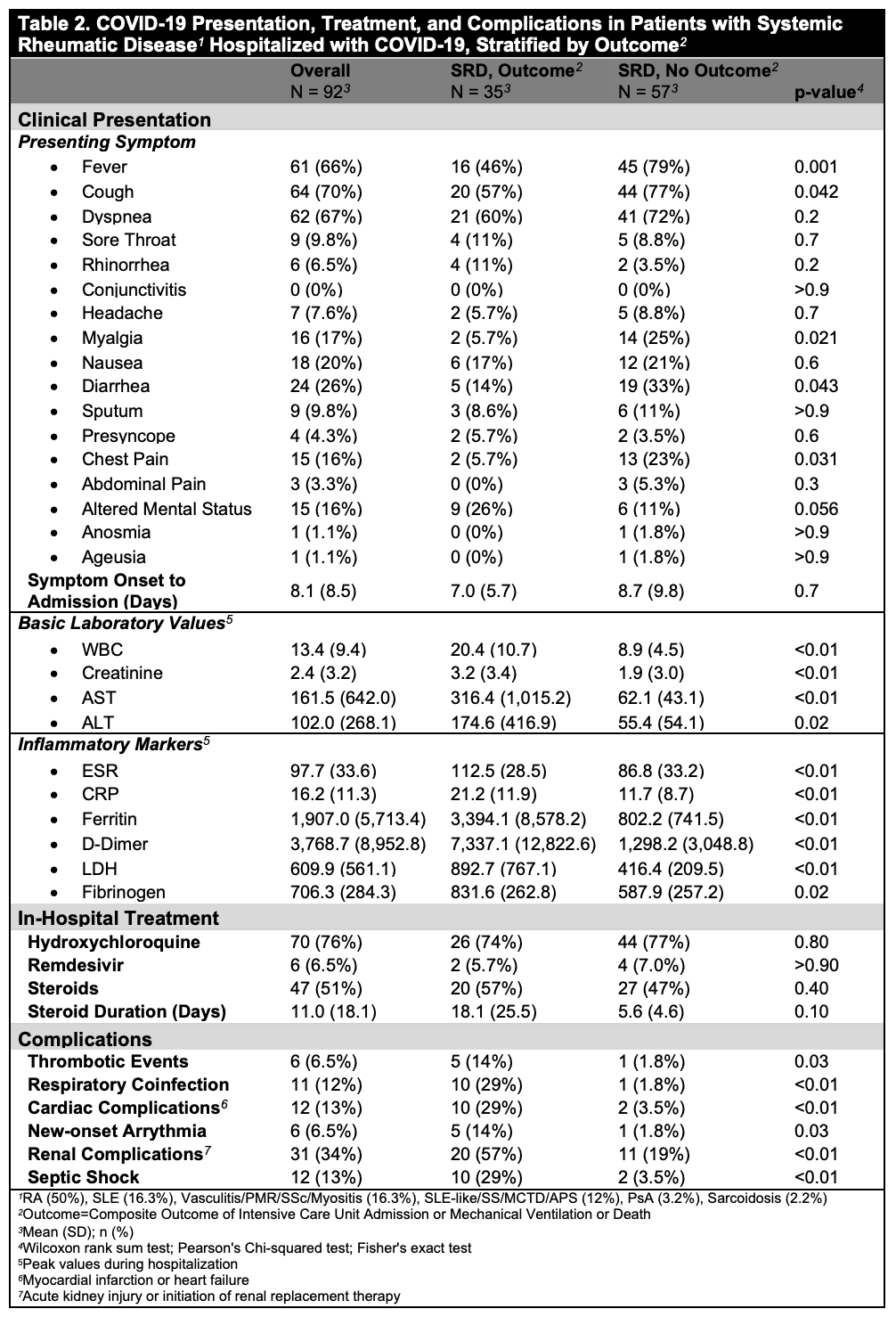
Results: Among 3,680 patients included in the NYP COVID-19 registry, 92 had an SRD (mean age 66.3 [16.5] years; 82% female, 40% White, and 26% Hispanic/Latinx; mean BMI 28.2 [6.7]). Patients with SRD and severe COVID-19 (N=35) were more likely to be older (73.5 [12.8] versus 61.8 [17.1] years), male, White or Asian, and have history of pulmonary disease or stroke compared to patients without severe COVID-19 (Table 1). No difference in baseline medications was noted. Both groups predominantly presented with fever and dyspnea, although the frequency of these symptoms was higher in the non-severe group (Table 2). Patients with SRD and severe COVID-19 had higher peak white blood cell count, creatinine, aspartate aminotransferase, and alanine aminotransferase levels; they also had higher peak inflammatory markers, including erythrocyte sedimentation rate, C-reactive protein, ferritin, D-dimer, lactate dehydrogenase, and fibrinogen (Table 2). There were no differences in in-hospital treatments. Thromboses, respiratory coinfections, septic shock, cardiac complications, and renal dysfunction were more common in patients with severe COVID-19 (Table 2).
Conclusion: Among SRD patients who were hospitalized for COVID-19 during the peak of the pandemic in New York City, demographic factors and medical comorbidities, but not baseline immunosuppressive medication use, were associated with severe COVID-19 leading to mechanical ventilation, ICU admission, or death. We were underpowered to perform subgroup analyses by SRD type. Future analyses are needed to evaluate the role of social determinants of health, access to care, and geocoding.
To cite this abstract in AMA style:
Siegel C, Choi J, D'Angelo D, Christos P, Lally L, Goyal P, Mandl L, Barbhaiya M. Characteristics Associated with Severe Outcomes in Patients with Systemic Rheumatic Diseases Hospitalized for COVID-19 in New York City [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/characteristics-associated-with-severe-outcomes-in-patients-with-systemic-rheumatic-diseases-hospitalized-for-covid-19-in-new-york-city/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-associated-with-severe-outcomes-in-patients-with-systemic-rheumatic-diseases-hospitalized-for-covid-19-in-new-york-city/