Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Psoriatic arthritis (PsA) is a common clinical feature in patients (pts) with psoriasis (PsO); up to one third of PsO pts will develop PsA in their lifetime.1 Despite this, the global Psoriasis and Beyond study, conducted by Novartis in partnership with IFPA, recently reported that 71% of PsO pts were unaware of the relationship between their skin disease and PsA. Here we describe the characteristics associated with a positive PEST score among PsO pts without a diagnosis of PsA from the Psoriasis and Beyond study.
Methods: Psoriasis and Beyond was a cross-sectional, quantitative online survey conducted in adults with a self-reported, physician-given diagnosis of moderate to severe PsO (body surface area [BSA] >5 to < 10% affecting sensitive and/or prominent body parts, or BSA ≥10%) at its worst, with/without concomitant PsA regardless of treatment. Pts without a confirmed diagnosis of PsA were screened using the Psoriasis Epidemiology Screening Tool (PEST); positive answers in ≥3 of 5 questions were considered as having a higher probability of undiagnosed PsA (ie, PEST-positive [PEST+] pts).
Results: A total of 4978 responses from 20 countries were analyzed; 3490 pts had a diagnosis of PsO only, while 1488 pts also had a diagnosis of PsA. Of the PsO only pts, 38% (n=1340) screened PEST+ (mean age, 41.3 years). Among pts with diagnosed PsA being PEST+, no difference regarding PsA severity between genders were reported. Women began to experience PsA symptoms at an average age of 32 years (29 years in men); however, more women reported morning stiffness (women vs men: 48% vs 33%).
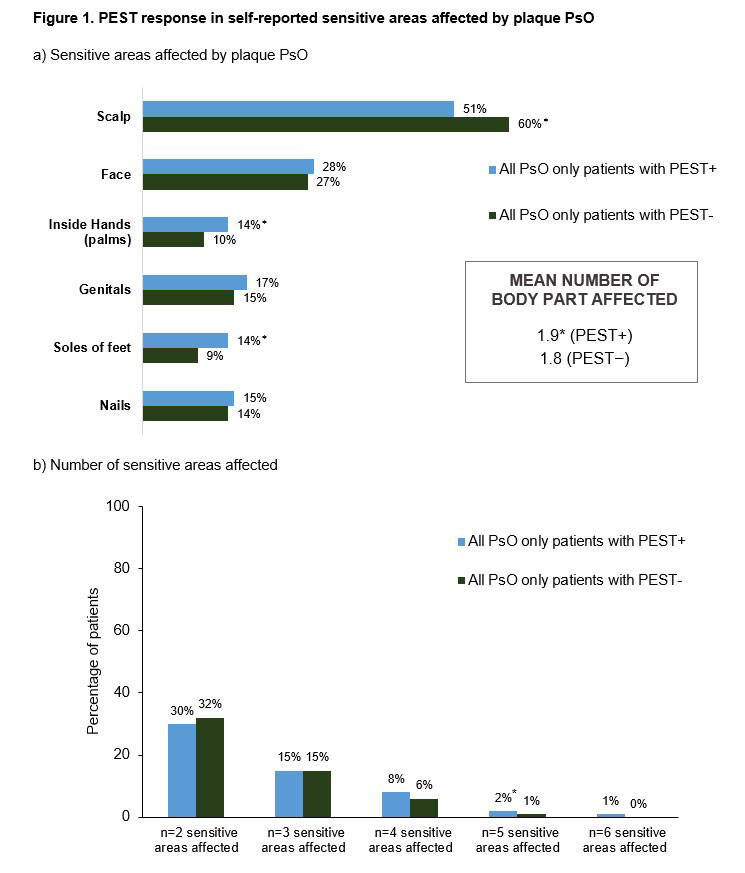
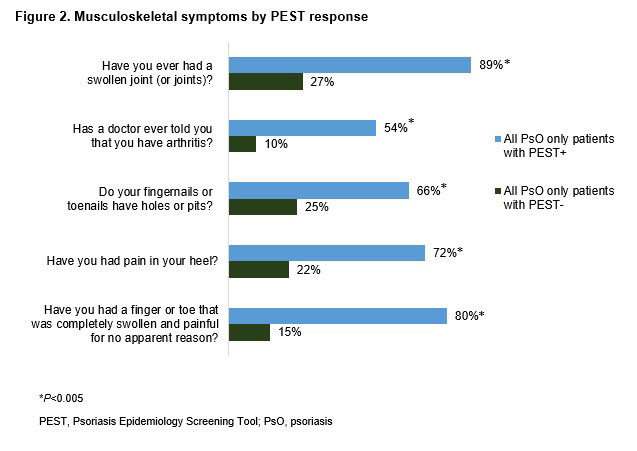
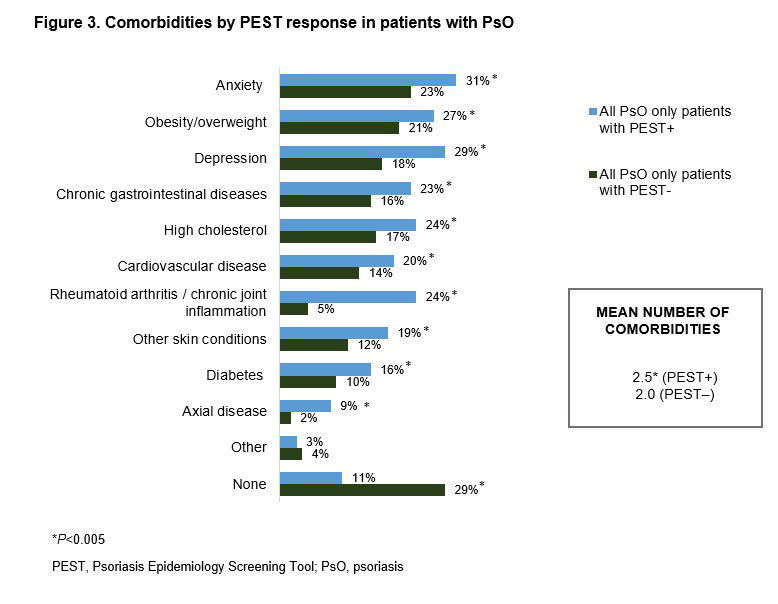
Of PEST+ pts without PsA diagnosis, PsO severity was categorized as moderate in 26% and severe in 13% of pts. Compared with PEST-negative (PEST−) pts, a higher proportion of PEST+ pts reported dry skin that may crack and bleed (57% vs 44%), soreness around psoriatic patches (36% vs 20%), and thick and pitted nails (16% vs 12%). Sensitive areas, including the palms and soles, were the most affected body parts reported by PEST+ pts (Figure 1). Regardless of the absence of PsA diagnosis, PEST+ (vs PEST−) pts reported having notably swollen joints (89% vs 27%), swollen finger(s) and/or toe(s) (80% vs 15%) and heel pain (72% vs 22%). The knees and hand/finger joints were the predominant joints causing discomfort for PEST+ pts (Figure 2). The comorbidity burden was higher in PEST+ pts with anxiety, depression, and obesity being the most commonly reported (Figure 3). PsO impact on quality of life was also substantial in PEST+ pts, with 38% and 26% of pts reporting a very large and extremely large effect on the patient’s life, compared with 22% and 5% of PEST− pts, respectively.
Conclusion: The analysis identified a large sub-population of PsO pts who screened PEST+, indicating a higher probability of having undiagnosed PsA and highlighting the need for active screening for PsA by the PsO-treating physicians to minimize non-reversible joint damage. Further, severe PsO and a high comorbidity burden may be associated with higher PEST scores. These associations should be further investigated in future studies.
Reference 1. Gottlieb, A., Merola J.F. J Dermatolog Treat. 2020;31:662–79.
To cite this abstract in AMA style:
Ogdie A, Armstrong A, Bohannan B, Mburu S, Coates L, Kornyeyeva E, Frade S, Fernandez Barrio S, Augustin M. Characteristics Associated with a Positive PEST Screening Among Patients with Psoriasis Without a Diagnosis of Psoriatic Arthritis: Results from the Global Psoriasis and Beyond Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/characteristics-associated-with-a-positive-pest-screening-among-patients-with-psoriasis-without-a-diagnosis-of-psoriatic-arthritis-results-from-the-global-psoriasis-and-beyond-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-associated-with-a-positive-pest-screening-among-patients-with-psoriasis-without-a-diagnosis-of-psoriatic-arthritis-results-from-the-global-psoriasis-and-beyond-study/