Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Calcinosis cutis is a debilitating complication of systemic sclerosis (SSc) affecting one quarter of patients, most frequently involving the hands. We previously developed and published a radiographic scoring system to assess severity of calcinosis affecting the hands in patients with SSc that is feasible with excellent inter- and intra-rater reliability. We sought to further validate our radiographic scoring system to assess for change over 1 year and to identify factors associated with improvement or progression.
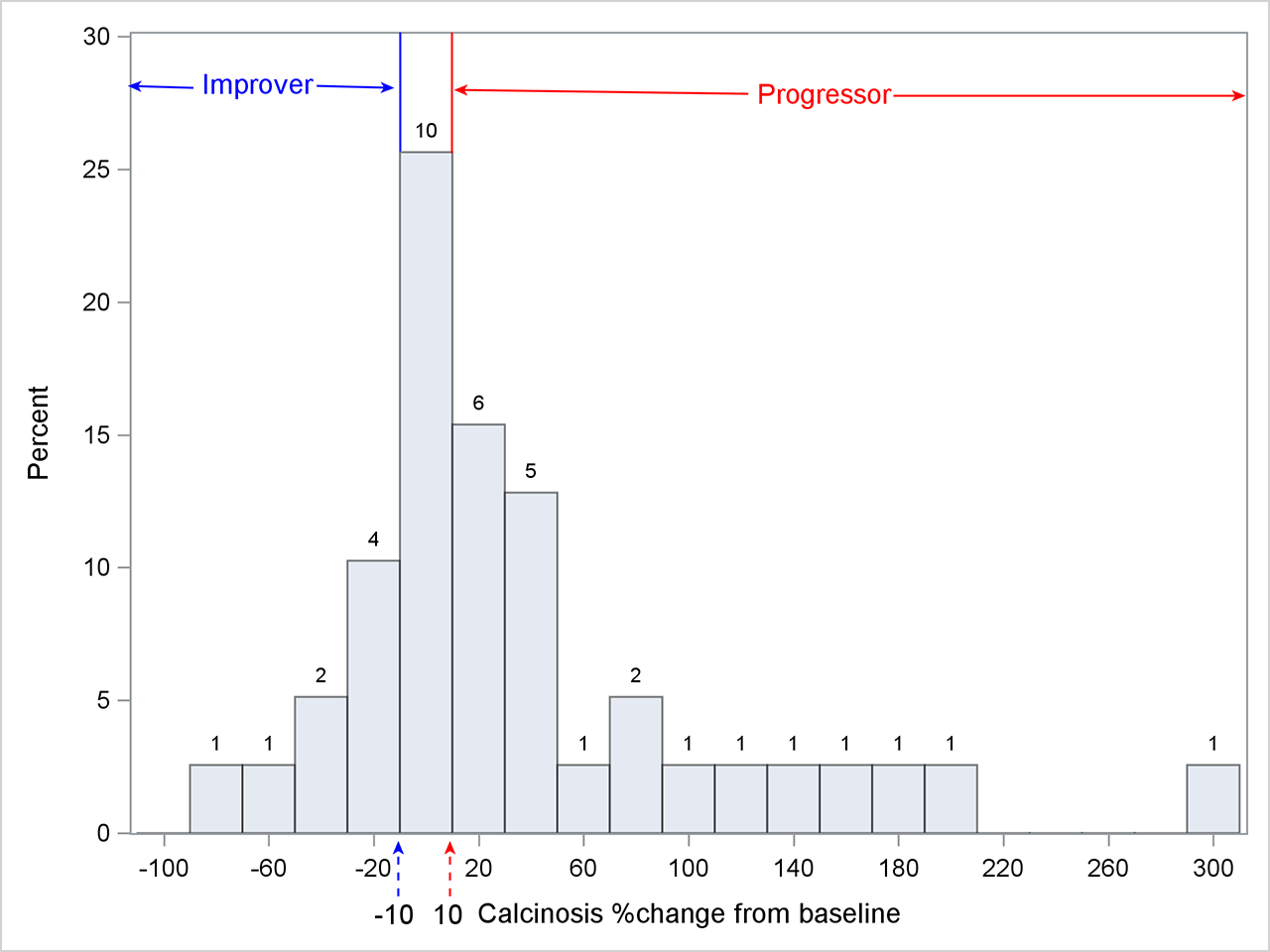
Methods: Baseline and 1-year antero-posterior hand radiographs were obtained in 39 SSc patients with calcinosis who were prospectively enrolled at 6 centers within the US, Canada, Mexico and Australia. Two blinded readers scored all radiographs using the calcinosis scoring system. We defined progressive calcinosis as >10% increase in score from baseline at 1 year, stable calcinosis as change in score between -10% to 10%, and improvement of calcinosis as decrease in score by >10% (Figure 1).
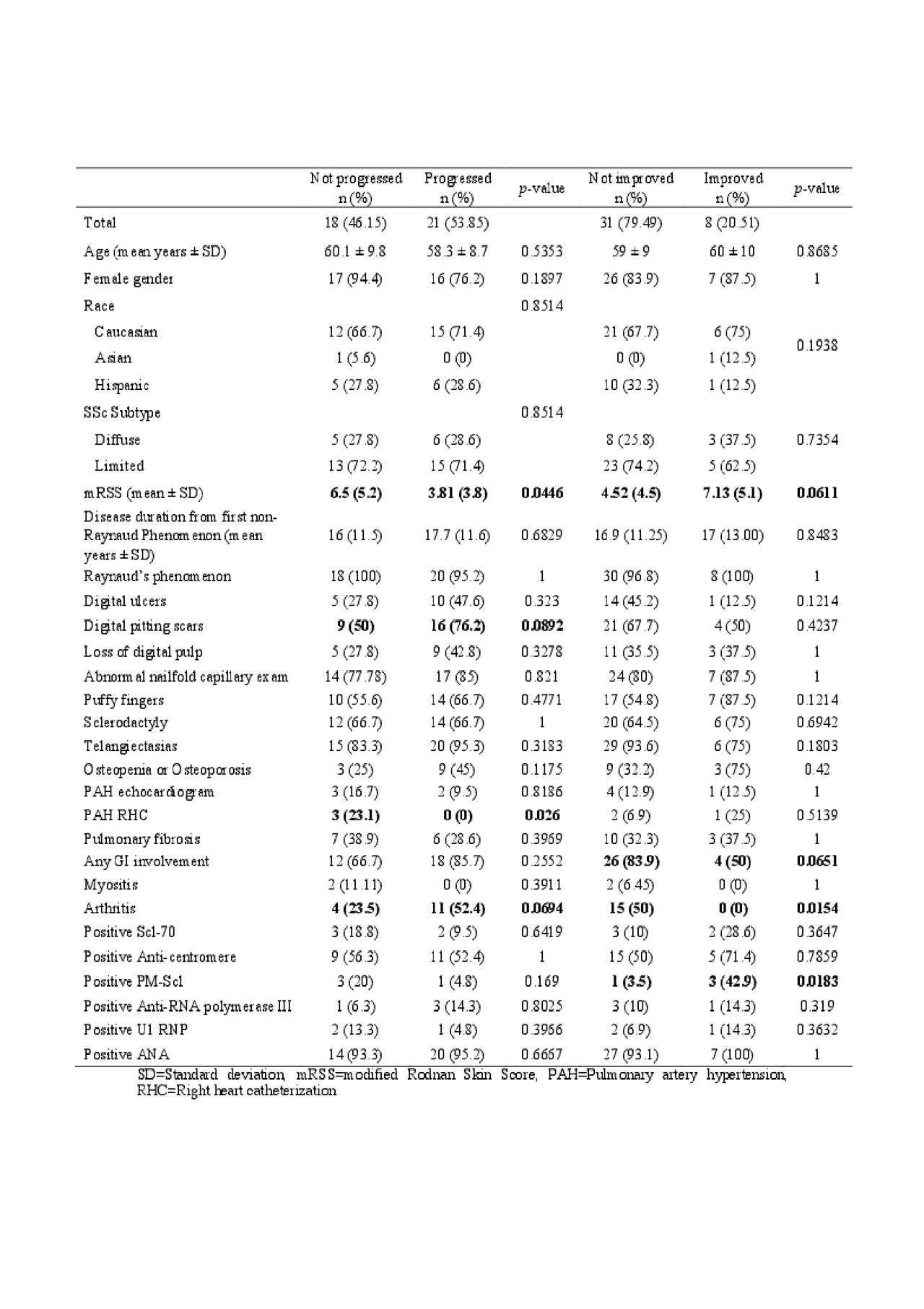
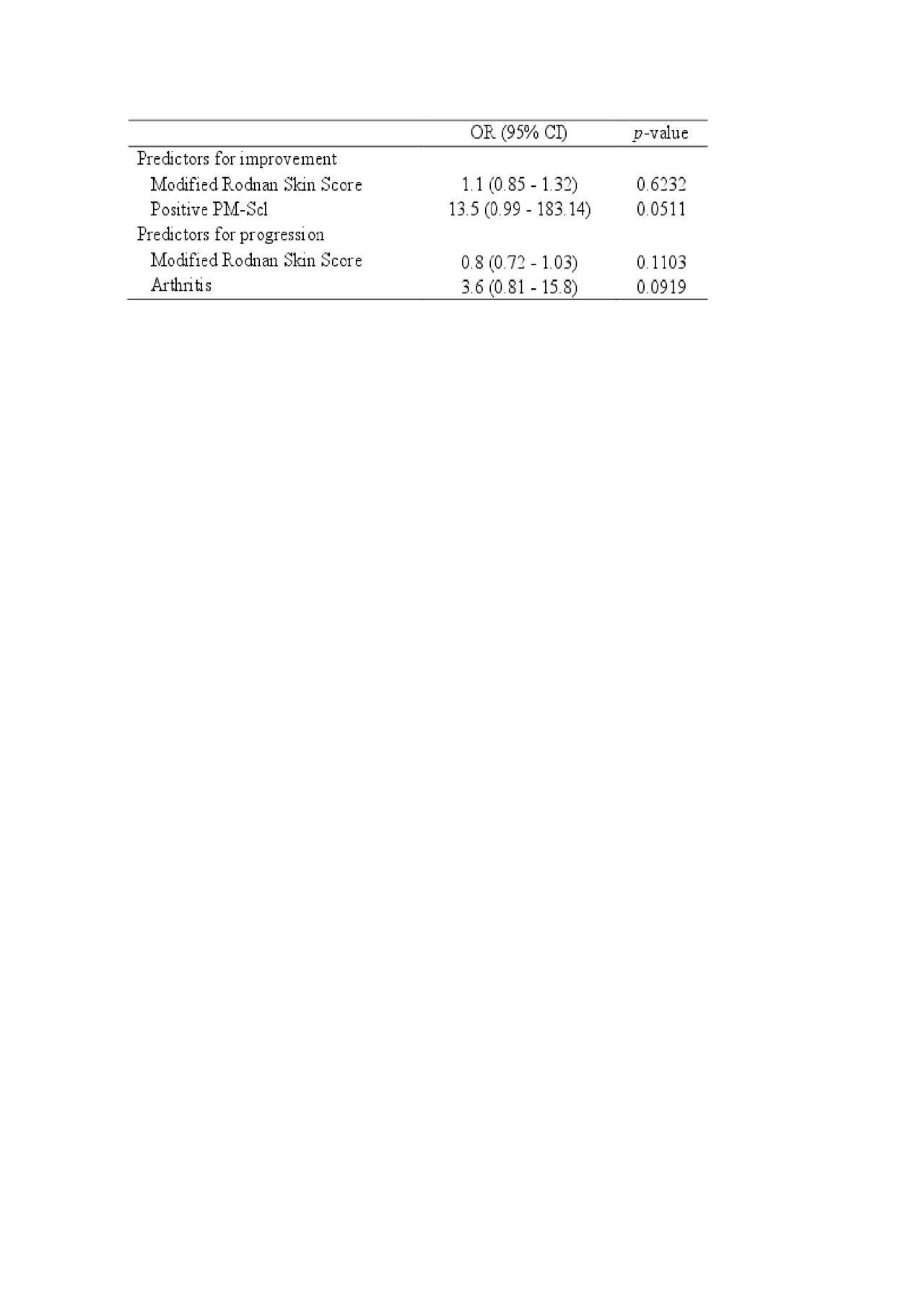
Results: Our cohort was 85% female, 69% Caucasian, 28% Hispanic, and 3% Asian. 72% had limited cutaneous disease. Mean disease duration from first non-Raynaud phenomenon (RP) symptom was 16.9±11.4 years. Inter-rater reliability was high with intra-class correlation coefficient of 0.93 (0.89-0.95). The median percentage of change from baseline to 1 year was 12.8% (range -89.3-290.2%). Twenty-one patients (54%) experienced progression of calcinosis over 1 year with a range of 12.7-290.2% worsening from baseline; 10 (26%) remained stable; and 8 (20%) had improvement (range -89.3-7.4%)(Figure 1). Patients with progressive calcinosis had lower mean modified Rodnan skin score (mRSS) (3.81 vs. 6.5, p=0.0446) and lower prevalence of pulmonary artery hypertension (PAH) by right heart catheterization than patients who did not progress (0 % vs 23%, p= 0.022)(Table 1). They also exhibited a trend toward having more digital pitting scars (76% vs. 50%, p= 0.0892), and arthritis (52% vs. 34%, p= 0.0694). Patients whose calcinosis improved had higher mean mRSS (7.13 vs. 4.52, p=0.061), less arthritis (0 vs. 50%, p=0.0154) and greater prevalence of antibodies against PM-Scl (43 vs. 3%, p=0.018) than patients whose calcinosis did not improve. They also exhibited a trend toward having less gastrointestinal disease (50 vs. 84%, p=0.0651). In multivariable analysis, a trend for anti-PM-Scl antibodies to be a predictor of calcinosis improvement persisted (OR 13.5 (0.99 – 183.14), p=0.051)(Table 2).
Conclusion: We confirmed the excellent inter-rater reliability of our radiographic calcinosis scoring system and quantified changes in calcinosis severity over 1 year in a longitudinal cohort of SSc patients. More than half of patients experienced >10% progression of calcinosis over one year; however, 20% of patients improved and these patients were more likely to be positive for the PM-Scl antibody.
To cite this abstract in AMA style:
Valenzuela A, Chung M, Rodríguez-Reyna T, Proudman S, Baron M, Castelino F, Hsu V, Li S, Fiorentino D, Stevens K, Chung L. Change in Calcinosis over 1 Year Using the SCTC Radiologic Scoring System for Calcinosis of the Hands in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/change-in-calcinosis-over-1-year-using-the-sctc-radiologic-scoring-system-for-calcinosis-of-the-hands-in-patients-with-systemic-sclerosis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/change-in-calcinosis-over-1-year-using-the-sctc-radiologic-scoring-system-for-calcinosis-of-the-hands-in-patients-with-systemic-sclerosis/