Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Despite effective control of inflammation, patients with rheumatoid arthritis (RA) may experience lingering pain and losses in physical function. Pain can occur because central nervous system (CNS) pain processing becomes dysregulated. Altered CNS pain regulation can lead to heightened pain perception and widespread pain sensitivity that may limit physical function. In this study, we examined associations between CNS pain regulation, pain intensity, and number of painful body sites with physical function during the early stages of RA. We hypothesized that abnormalities in CNS pain regulation, higher pain intensity, and a greater number of painful body sites would be associated with lower physical function in patients with early RA.
Methods: Cross-sectional baseline data were analyzed from adults with early RA enrolled in the on-going Central Pain in RA 2 (CPIRA-2) study. Eligible participants met the ACR/EULAR 1987 or 2010 criteria for RA, had persistent joint symptoms for ≤ 24 months, and active disease. Physical function was assessed by the PROMIS physical function questionnaire, which measures functional capability of different body regions and activities of daily living. Quantitative sensory tests (QST), including pressure pain threshold (PPT), temporal summation (TS), and conditioned pain modulation (CPM), were performed to assess mechanisms of CNS pain regulation. PPT measures overall pain sensitization, while TS and CPM assess ascending (pain facilitation) and descending (pain inhibition) analgesic pathways, respectively. Pain intensity was assessed using a 0-10 numeric rating scale, and the number of painful body sites was assessed using the CHOIR body map. Spearman’s correlations were computed to examine bivariate associations between each pain measure and physical function. Separate linear regression models estimated unadjusted and adjusted associations between each QST measure, pain intensity, number of painful body sites, and physical function, adjusting for age, sex, body mass index (BMI), and swollen joint count.
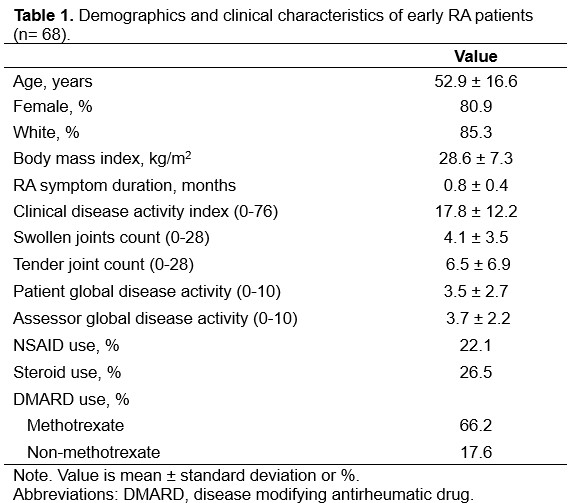
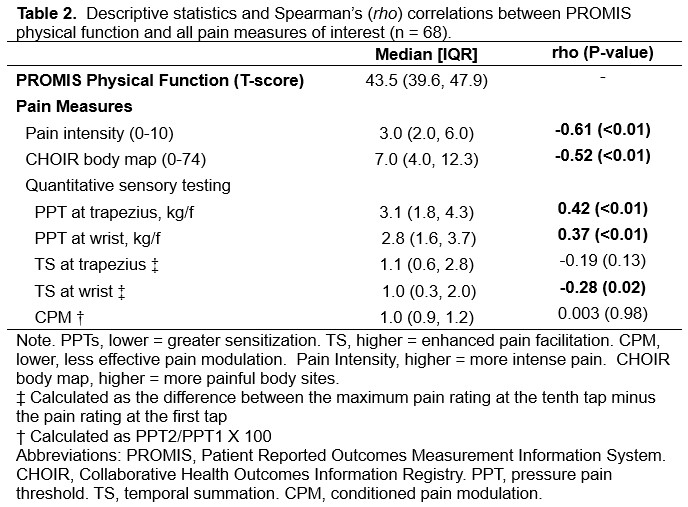
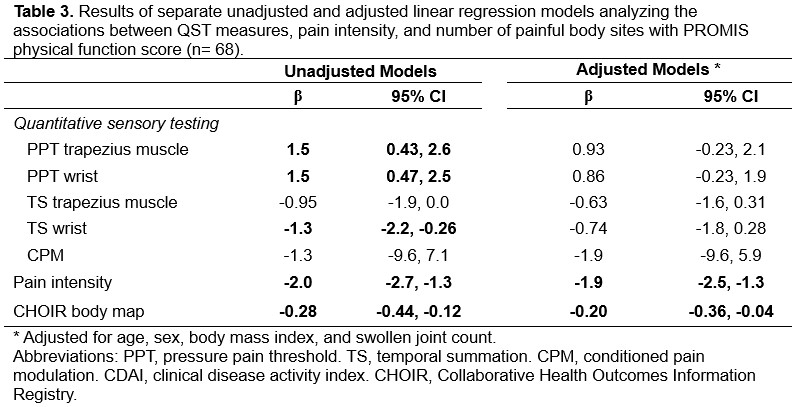
Results: Our sample included 68 patients (81% female, 85% white) with mean (SD) age of 52.9 (16.6) years, BMI of 28.6 (7.3) kg/m2, and RA symptom duration of 0.8 (0.4) months (Table 1). Approximately 65% had mild to severe functional limitations (t-score ≤ 45). Higher PPTs (trapezius and wrist), lower TS at the wrist, greater pain intensity, and more painful body sites were each associated with lower physical function (Table 2). In adjusted models, greater pain intensity (β = -1.9 [95% CI -2.5 to -1.3]) and more painful body sites (β = -0.20 [95% CI -0.36 to -0.04]) remained significantly associated with poor physical function (Table 3).
Conclusion: Among patients with early RA, a phenotypic pain profile comprised of high pain sensitization, high pain intensity, and many painful body sites was associated with poor physical function. Incorporating pain management strategies in patients with early RA may help them maintain physical function. Longitudinal work is needed to explore causal pain pathways and identify interventions that may be in addition to DMARD therapy to improve long-term physical function and quality of life related to pain pathways.
To cite this abstract in AMA style:
Aydemir B, Muhammad L, Song J, Dunlop D, Aren K, Carns M, Marder W, Bykerk V, Deane K, Bingham C, Lee Y. Central Pain Mechanisms and Physical Function in Early Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/central-pain-mechanisms-and-physical-function-in-early-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/central-pain-mechanisms-and-physical-function-in-early-rheumatoid-arthritis/