Session Information
Date: Tuesday, November 14, 2023
Title: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular (CVD) comorbidity can impact overall RA care. We demonstrated that CVD risk factors were associated with higher disease activity and disability. Here, we investigated whether CVD risk factors reduce treatment response by influencing retention of a first biologic disease-modifying antirheumatic drug (bDMARD) or targeted synthetic DMARD (tsDMARDs).
Methods: Participants enrolled in the Ontario Best Practices Initiative (OBRI) RA registry were included if they initiated their first bDMARD or tsDMARD. They were grouped by the number of baseline CVD risk factors (0, 1 or ≥2) including hypertension, dyslipidemia, diabetes, obesity and current smoking. The primary outcome was time-to-discontinuation of therapy for any reason. Secondary outcomes included discontinuation for primary failure, secondary failure or due to adverse events. Multivariable Cox proportional hazards model, adjusted for clinically important confounders, estimated the association between CVD risk factors and drug retention.
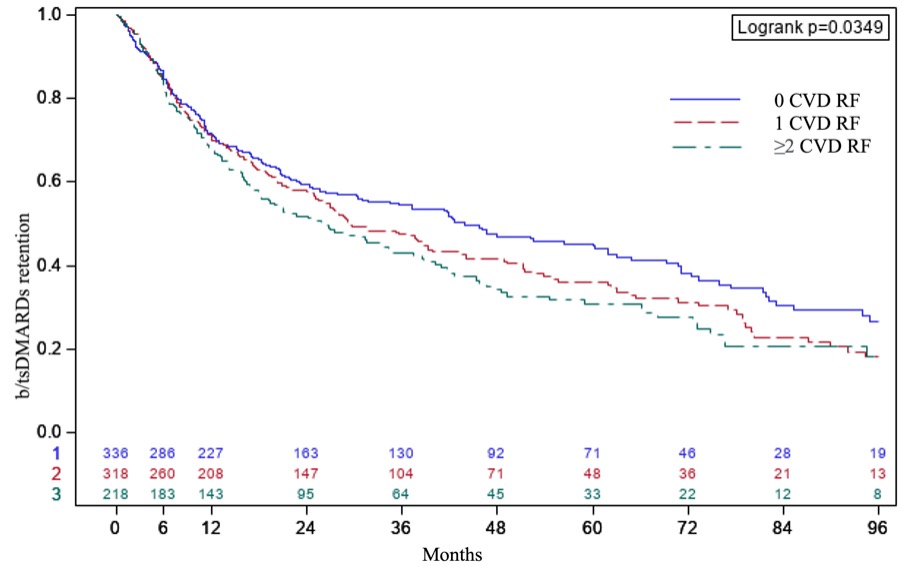
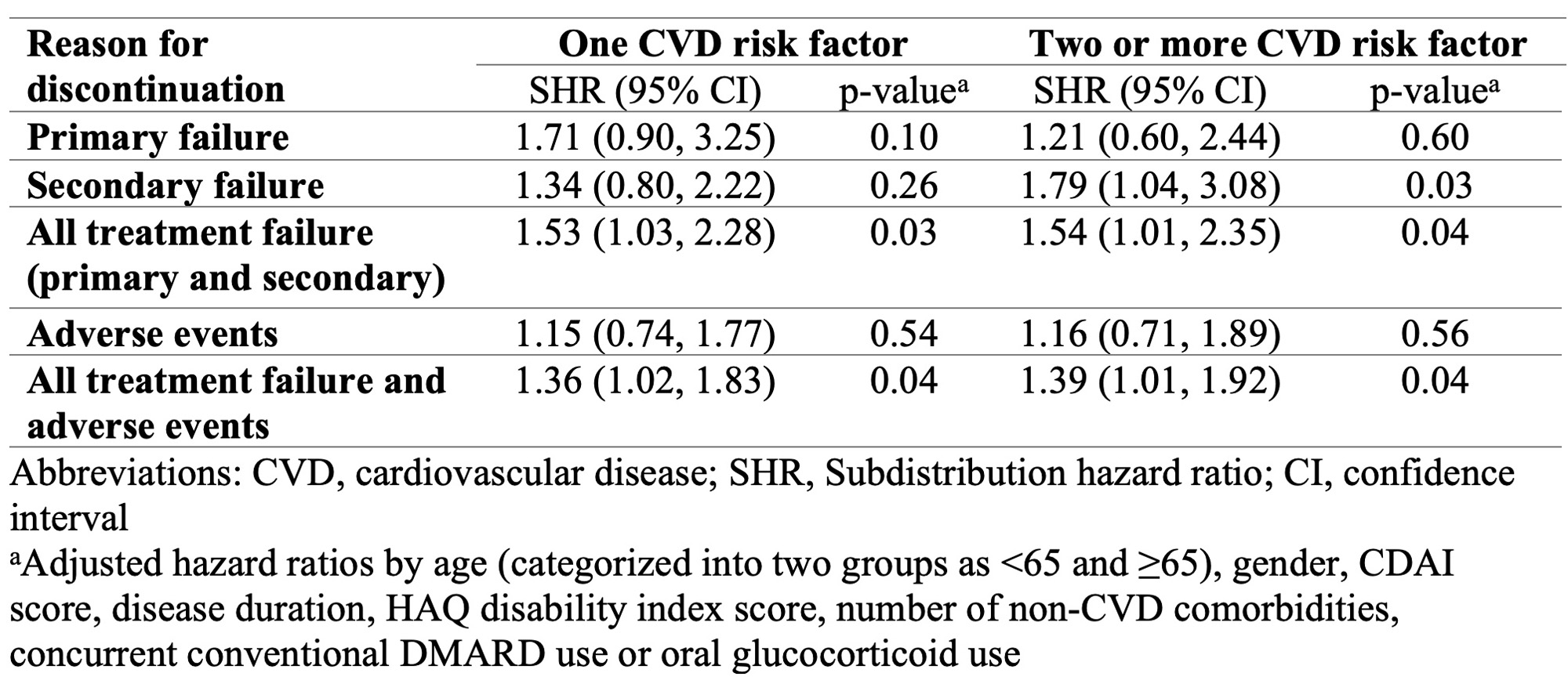
Results: A total of 872 patients were included, of which 62% had at least one CVD risk factor. The baseline characteristics are described in Table 1. Fifty-eight percent (N=508) of the study population discontinued their initial b/tsDMARD after a median of 13 (interquartile range [IQR], 6 to 29) months. The most common causes for treatment discontinuation were primary failure (N=72), secondary failure (N=126), and adverse events (N=133). Patients with no CVD risk factors experienced longer drug survival, with a median (IQR) duration of 44 months (30 to 62). In contrast, patients with 1 or ≥2 CVD risk factors had significantly shorter drug survival, averaging 29 (IQR 25 to 39) and 26 (IQR 18-34), respectively (p= 0.03). Compared to patients with no CVD risk factors, only patients with ≥2 CVD risk factors had a significant increase in all-cause discontinuation: HR 1.32 (95% CI 1.07, 1.65, p= 0.01). In multivariate-adjusted analysis, no significant association was found between all-cause discontinuation and CVD risk factor status. However, there was a significant association between the presence of >1 CVD risk factor and drug discontinuation, notably for secondary failure (Table 2).
Conclusion: The presence of multiple CVD risk factors increases the risk of treatment failure, primarily secondary failure, among biologic naïve patients starting their first advanced therapy. Future research is needed to explore the effect of interventions aiming at reducing these modifiable risk factors on the response to targeted therapies.
To cite this abstract in AMA style:
Aboulenain S, Li X, Movahedi M, Bombardier C, Kuriya B. Cardiovascular Risk Factors Are Associated with Discontinuation of Advanced Therapies Due to Treatment Failure in Rheumatoid Arthritis: Results from the OBRI [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-risk-factors-are-associated-with-discontinuation-of-advanced-therapies-due-to-treatment-failure-in-rheumatoid-arthritis-results-from-the-obri/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-risk-factors-are-associated-with-discontinuation-of-advanced-therapies-due-to-treatment-failure-in-rheumatoid-arthritis-results-from-the-obri/