Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: A growing body of evidence highlights a link between rheumatic diseases such as rheumatoid arthritis (RA), psoriatic arthritis (PA), and systemic lupus erythematosus (SLE) and an increased risk of cardiovascular events (CVE). Investigating this relationship and the specific risk factors associated with CVE in this population is vital for early identification, prevention and risk stratification. The objective of this study was to identify risk factors for CVE in RA, SLE, and PSA members.
Methods: This was a cohort study of commercial fully-insured and Medicare Advantage members of a large national health plan between 1/1/2018 and 1/1/2024. Members ≥ 18 years old were included if they had at least 2 claims for RA (ICD-10 code: M05 or M06), PSA (L40.5), or SLE (M32) during the evaluation period; members with a prior MI or ischemic stroke were included. Members were excluded if they did not maintain continuous eligibility for 6 months before or after entrance into the analysis, had multiple conditions of interest (RA, PSA, or SLE), or had missing socioeconomic status (SES) data. The primary outcome was incidence of CVE defined by ICD-10 codes for myocardial infarction (MI; I21.X, I22.X, I23.X) or ischemic stroke (I63.X, I64.X). Member demographics, social determinants of health (SDoH), and comorbidities were analyzed for those with CVE and those without. Continuous variables were assessed with an independent t-test or Mann-Whitney U test; categorical variables were assessed with a ꭓ2 test. Bivariate and multivariate Poisson regression was utilized to identify correlations between variables and CVE rates; p-values < 0.05 were significant.
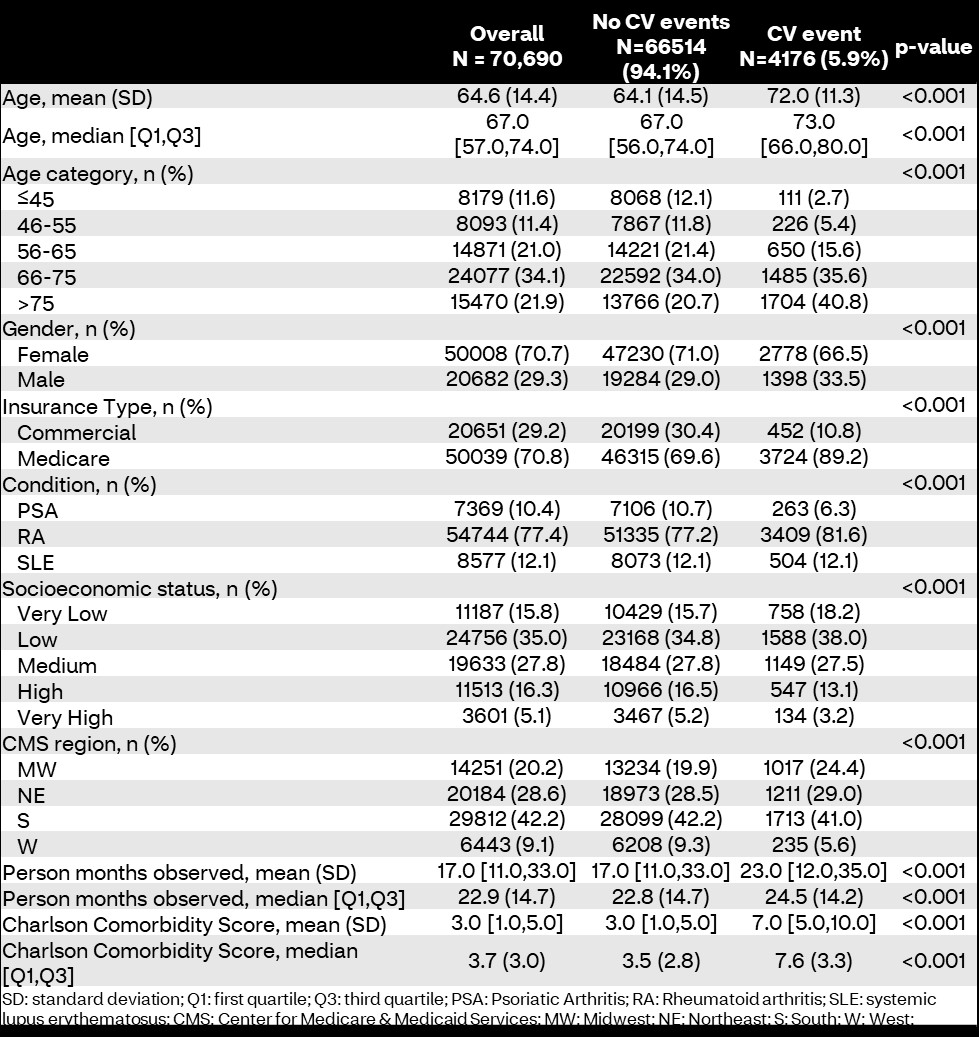
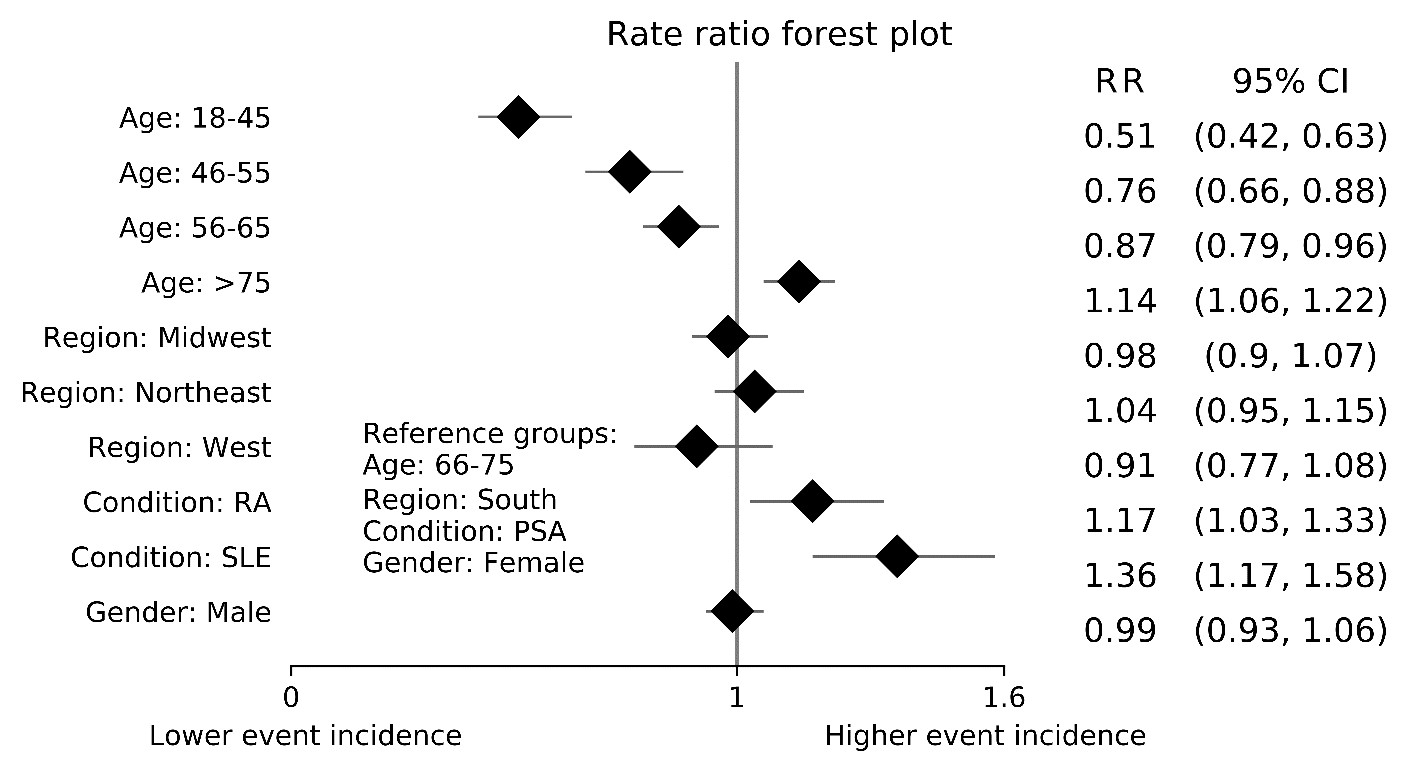
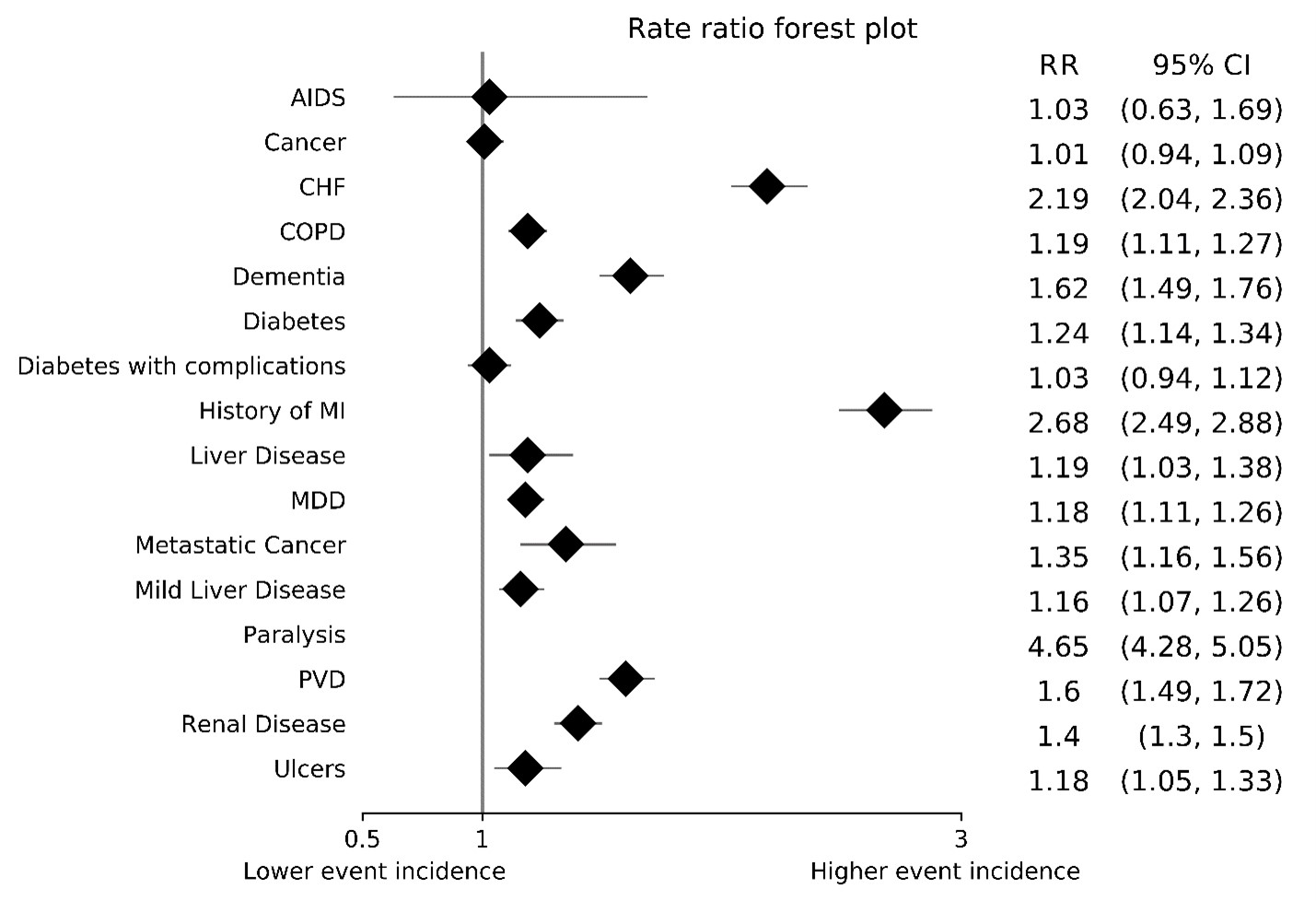
Results: 70,690 members were included with 4,176 (5.9%) experiencing a CVE during the evaluation period or 30.9 cases per 1,000 person-years (PY) observed. Among the conditions of interest, PSA had lower incidence rates than RA and SLE (18.8 [16.6-21.2] cases/1,000 PY vs. 32.6 [31.5-33.7] and 30.7 [20.1-33.5] cases/1,000 PY, respectively; p< 0.001 for both comparisons). Members experiencing CVE were older, (66+ years of age) more likely to be male, have Medicare insurance, have lower SES, and with more comorbidities (Table 1). CVE incidence risk increased with age, with lowest risk being in members aged 18-45 years and highest being in members aged >75 years (Figure 1). Comorbidities associated with increased CVE risk include history of MI, congestive heart failure, dementia, peripheral vascular disease, renal disease, AIDS, diabetes mellitus, metastatic cancer, depression, liver disease, ulcers, and congestive obstructive pulmonary disease (Figure 2). SDoH factors were not associated with CVE risk in the final multivariate model.
Conclusion: In this evaluation of a population of members with elevated CVE risk, factors associated with CVE appear to parallel those seen in other high-risk populations, namely increasing age, and chronic comorbidities. SDoH factors were not associated with CVE incidence; however, additional investigation is warranted.
To cite this abstract in AMA style:
Park J, Rutter C, Avalos-Reyes E, Anderson M, Cavers W, Verbrugge D, Johnson K. Cardiovascular Event Risks Among Members with Rheumatoid Arthritis, Psoriatic Arthritis, and Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-event-risks-among-members-with-rheumatoid-arthritis-psoriatic-arthritis-and-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-event-risks-among-members-with-rheumatoid-arthritis-psoriatic-arthritis-and-systemic-lupus-erythematosus/