Session Information
Date: Saturday, November 6, 2021
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Cardiovascular Pulmonary Disease (0268–0295)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with inflammatory rheumatic diseases such as rheumatoid arthritis (RA), psoriatic arthritis (PsA) and ankylosing spondylitis (AS) are at a higher risk for developing cardiovascular diseases (CVD) than the general population. This increased risk is partly due to a higher incidence of traditional cardiovascular (CV) risk factors, such as hypertension and dyslipidemia, and partly due to the underlying systemic inflammation. During the past two decades, the burden of the systemic inflammation has been reduced by more efficacious anti-inflammatory treatment, which somewhat attenuated the increased CV risk of rheumatic patients. However, it remains important to monitor the effects of these new treatment strategies on the prevalence of CVD in patients with a rheumatic disease in systematically controlled cohorts.
The aim of the current report was to evaluate whether the CV risk of patients with inflammatory rheumatic diseases still differs from the general population, despite advances In anti-rheumatic treatment strategies.
Methods: In March 2020, all adult patients with an inflammatory rheumatic disease from the Amsterdam Rheumatology and Immunology Center, location “Reade” were systematically asked to participate in a prospective cohort study. The primary aim of this study was to monitor the impact of the COVID-19 pandemic on patients with inflammatory rheumatic diseases compared to age and sex matched healthy controls. Between April 26, 2020 and May 27, 2020, participants completed the first online questionnaire of the study. Amongst others, information on demographic data, including CV comorbidities and risk factors, and medication use was collected. The baseline characteristics and prevalence of CVD were compared between RA, PsA or AS and healthy controls.
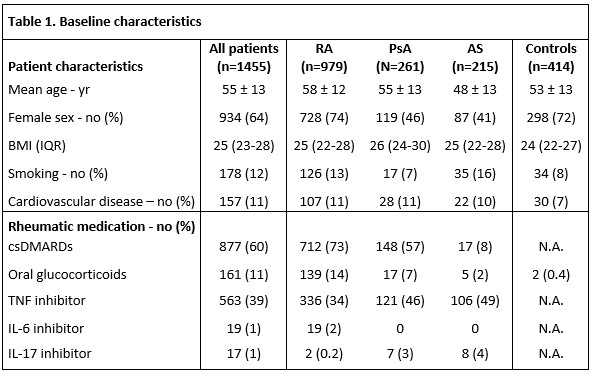
Results: In total, 1455 consecutive patients with an inflammatory rheumatic disease (979 RA patients, 261 PsA patients and 215 AS patients), and 414 healthy controls completed the first questionnaire, as shown in table 1. CV comorbidities were more frequently reported in RA, PsA and AS patients compared to healthy controls; 107 (11%), 28 (11%) and 22 (10%) compared to 30 (7%), respectively. Unadjusted odds ratios with corresponding 95%-confidence intervals for patients with RA, PsA and AS compared to controls were 1.57 (1.03-2.40), 1.54 (0.90-2.64) and 1.46 (0.82-2.60).
Conclusion: We demonstrated that the prevalence of CVD is approximately 1.5 times higher in patients with rheumatic diseases compared to healthy controls (11% vs. 7%, respectively). This corresponds with previous research, although the reported prevalence of CVD in PsA and AS patients is even higher compared to prior studies. This suggests that the CVD risk of patients with rheumatic diseases is still elevated in 2020 compared to the general population, despite the improved management of rheumatic disease activity. Therefore, adequate and timely treatment of CV risk factors remains relevant, not only in patients with RA, but in patients other rheumatic diseases as well.
To cite this abstract in AMA style:
Raadsen R, Hooijberg F, Boekel L, Vogelzang E, Wolbink G, Lems W, van Kuijk A, Nurmohamed M. Cardiovascular Disease Risk in Inflammatory Arthritis Patients Still Substantially Elevated in 2020 [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-disease-risk-in-inflammatory-arthritis-patients-still-substantially-elevated-in-2020/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-disease-risk-in-inflammatory-arthritis-patients-still-substantially-elevated-in-2020/