Session Information
Date: Sunday, November 12, 2023
Title: (0691–0721) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular disease (CVD) is the leading cause of death in patients with the most common subtypes of primary systemic vasculitides. We aimed to estimate the scope of cardiovascular-related death in patients with primary systemic vasculitis in the United States in recent years.
Methods: We used the CDC Wonder Multiple Causes of Death database and its query system. All deaths related to cardiovascular disease (CVD) as the UCD, and primary systemic vasculitides as CCDs were included from January 1, 1999, to December 31, 2020. We used the ICD-10 code I00-I99 (Diseases of the circulatory system) as the UCD, and the ICD-10 codes of the different subtypes of the primary systemic vasculitides were grouped as CCDs. Diseases of the circulatory system and all grouped vasculitides were initially queried separately, and the 2 disorders were also queried together to find out the mortality rates of CVD as UCD and vasculitis as CCD. We also performed the analysis by vasculitis subtypes. We obtained mortality rates by year, gender, race, and state. To obtain age-adjusted mortality rates we used the year 2000 U.S. standard population. We show mortality rates as the number of deaths per 100,000 for CVD, and per million for vasculitis. We applied a linear regression model to evaluate trends over time.
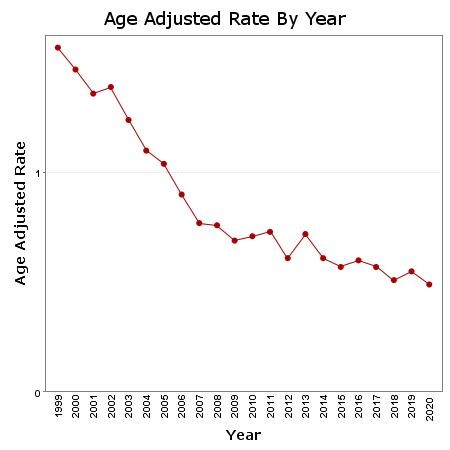
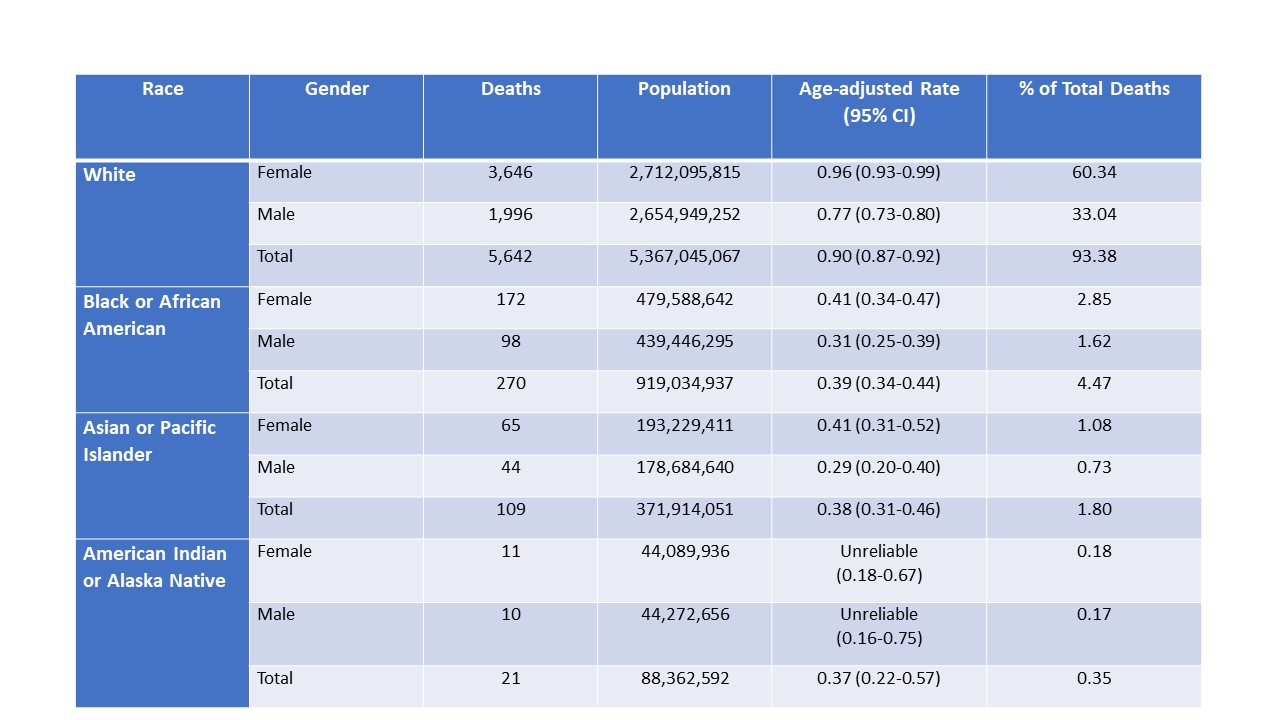
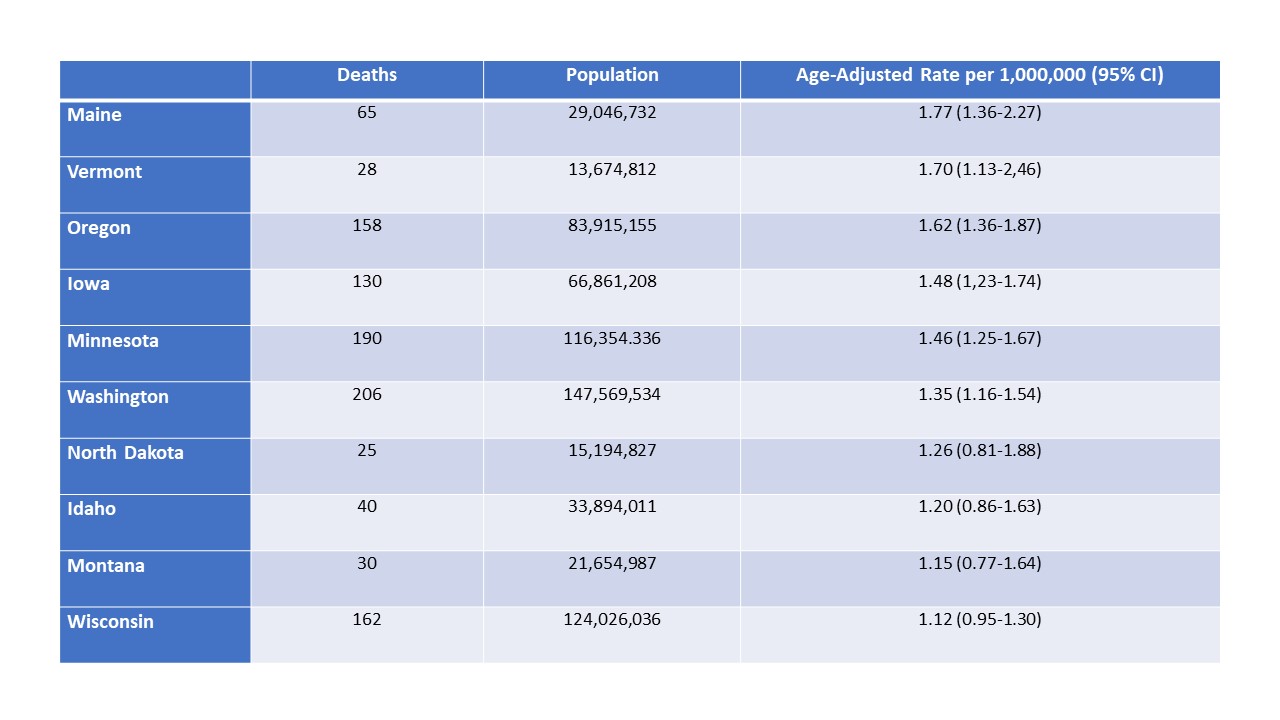
Results: During the 22-year period, CVD was the UCD of death of 18,783,791 patients. The age-adjusted mortality rate was 254.38 per 100,000 (95% CI: 254.27-254.50). For vasculitis as CCD, there were 29,229 deaths, and the age-adjusted mortality rate was 4.02 per 1,000,000 (95% CI: 3.97-4.07). When CVD as UCD and vasculitis as CCD were combined, there were 6,042 deaths, with an age-adjusted rate of 0.82 per 1,000,000 (95% CI: 0.80-0.84). Since 1999, there has been a significant trend to the decrease (p< 0.0001) (Figure 1). The age-adjusted mortality rate was higher in females than in males (0.88 vs. 0.71 per million). The percentage of females was 64.5%. The age-adjusted mortality rate was higher in Whites (0.90, 0.87-0.92) than in Blacks (0.39, 0.34-0.44) (Table 1). The percentage of Whites was 93.4%. M31.6 (Other giant cell arteritis) accounted for 58% of all vasculitis deaths. There was differential geographic distribution in the mortality rates by state. The states with the highest age-adjusted mortality rates were Maine, Vermont, Oregon, Iowa, and Minnesota (Table 2). The states with the lowest rates were Louisiana, Nevada, Mississippi, Florida, and Georgia.
Conclusion: There has been a progressive decrease in mortality rates in recent years. Contrary to what is found in the general population, in our study, the age-adjusted mortality rates were higher in females and in Whites. This can be explained, at least in part, by the fact that vasculitides are more frequent in Whites, and GCA, which is the subtype of vasculitis associated with the highest mortality rate in our study, is more frequent in white females. Mortality rates of vasculitis are more frequent in northern states. Investigation of the reasons for the geographic disparities is warranted. Our findings should be taken with caution until quality studies to determine the reliability of the data about these rare diseases available in national databases are performed.
To cite this abstract in AMA style:
Rodriguez-Pla A. Cardiovascular Disease-Related Mortality in Primary Systemic Vasculitis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-disease-related-mortality-in-primary-systemic-vasculitis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-disease-related-mortality-in-primary-systemic-vasculitis/