Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Insomnia is a significant challenge for rheumatoid arthritis (RA) patients. Chronic pain conditions often exacerbate sleep disturbances, creating a vicious cycle where pain and sleep deprivation perpetuate each other with pain not only interrupting sleep but also causing poor sleep quality contributing to increased pain sensitivity. Insomnia exacerbates the pain and fatigue associated with RA, further diminishing physical function and psychological well-being. Despite this, the prevalence and impact of insomnia in RA patients remain under-recognized and under-treated. The aim of this work is to identify the frequency of insomnia in RA patients, highlighting the necessity for more research, increased awareness, and targeted therapeutic interventions.
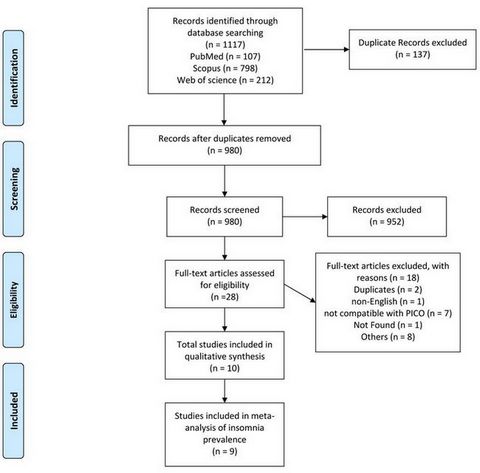
Methods: We systematically searched PubMed, Web of Science, and Scopus databases from inception till January 20, 2024. Adhering to PRISMA guidelines1 (Figure 1), we screened and assessed the methodological quality of eligible studies, including only those of high quality. Statistical analysis included meta-analysis utilizing both random and fixed effects models to estimate pooled insomnia prevalence, accounting for variations in the study populations, and potential publication bias in the analyses using Jamovi 2.3.21.0.
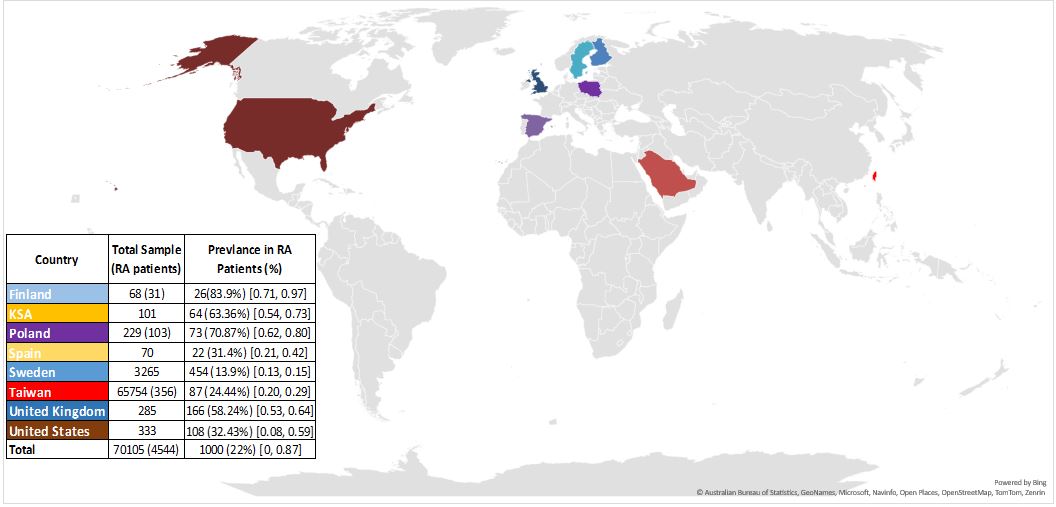
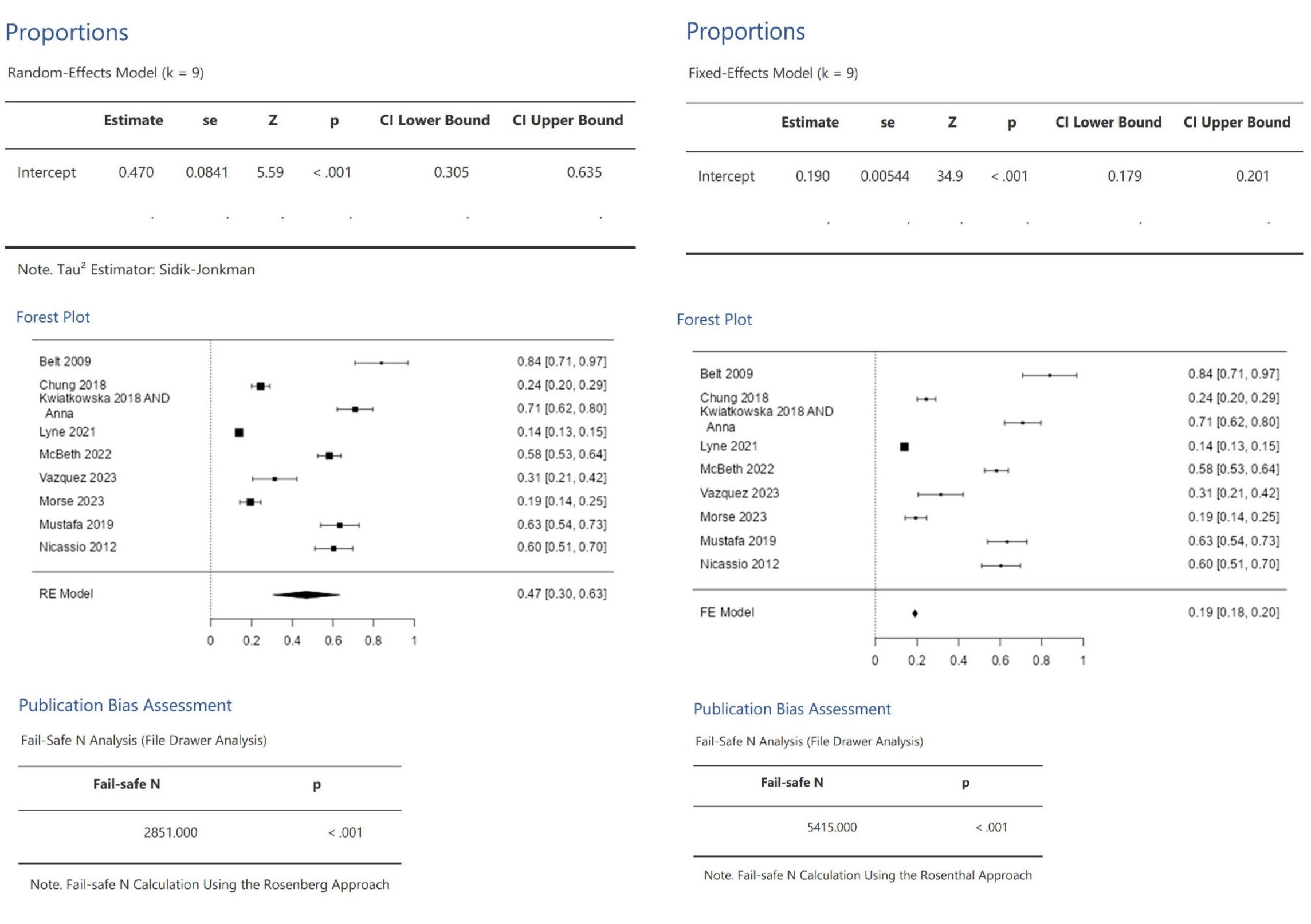
Results: The literature search yielded 1,117 articles, we included nine studies that reported prevalence of insomnia cases within RA patients, incidence of new cases, or both. We identified diverse designs: three studies were cross-sectional, three were case-control studies, and three were cohort studies. Twenty-two percent of RA patients experienced insomnia (Figure 2), significantly surpassing the general population prevalence of 5.6%2. Sample size median and range 227 (68 to 65,754). Utilizing both random and fixed effects models in our analysis, the aggregated random effects analysis revealed an insomnia prevalence of 47% (95% CI: 0.305 to 0.635) across nine studies, encompassing 70,105 patients (Figure 3). The pooled fixed effects estimate for insomnia prevalence was 19.0% (95% CI: 0.190 to 0.201). The fail-safe N analyses are (2851 (P< 0.001) and 5415 (P< 0.001)) for random and fixed effects models, respectively, Suggesting that the observed effect sizes are robust and unlikely to be influenced by publication bias. Global distribution showed that Sweden had the lowest prevalence (13.9%) [95% CI:0.13, 0.15] in Fixed-effect model.
Conclusion: This is the first systematic review and meta-analysis of insomnia prevalence in RA patients, revealing that RA patients are four times more likely to experience insomnia than the general population, emphasizing the need for heightened awareness among RA patients and healthcare providers. These findings highlight crucial gaps in the current understanding of insomnia in RA, advocating for further research in this area.
References
1-Takkouche B, Norman G. PRISMA statement. Epidemiology. 2011 Jan 1;22(1):128.
2- Øverland S, Ursin R, Tell GS, Salo P, Bjorvatn B, Glozier N, Pallesen S, Sivertsen B. Midlife insomnia and subsequent mortality: the Hordaland health study.
(Fail safe N = 2851.0, p < 0.001) and (Fail safe N = 5415.0, p < 0.001).
Estimate: The value of the intercept in the model, se (Standard Error), Z (Z-value), p (p-value), CI (Confidence Interval).
To cite this abstract in AMA style:
Abdelsalam M, Khairy M, Awad M, Alnabawy A, Taha M, Al-Adl Ali Ali M. Can’t Sleep, Won’t Sleep: A Systematic Review and Meta-Analysis of Insomnia Prevalence in 70,105 Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/cant-sleep-wont-sleep-a-systematic-review-and-meta-analysis-of-insomnia-prevalence-in-70105-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cant-sleep-wont-sleep-a-systematic-review-and-meta-analysis-of-insomnia-prevalence-in-70105-rheumatoid-arthritis-patients/