Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The increased cancer risk in patients with systemic lupus erythematosus (SLE) has received considerable attention. However, there is a lack of studies examining the cancer risk in newly diagnosed SLE patients, and the estimation of risk factors remains inadequate. This study aims to profile cancer incidence and identify risk factors in patients with newly diagnosed SLE.
Methods: From 2008 to 2018, all incident SLE patients were recruited from a comprehensive dataset combining information from the National Health Insurance Service, Health Insurance Review & Assessment Service, and Korea Central Cancer Registry. The study calculated the incidence rates (IRs) per 1,000 person-years (PYs) for site-specific cancers using the Surveillance, Epidemiology, and End Results (SEER) stage classification. Multivariable logistic regression analysis was employed to determine the association between incident SLE patients and risk factors.
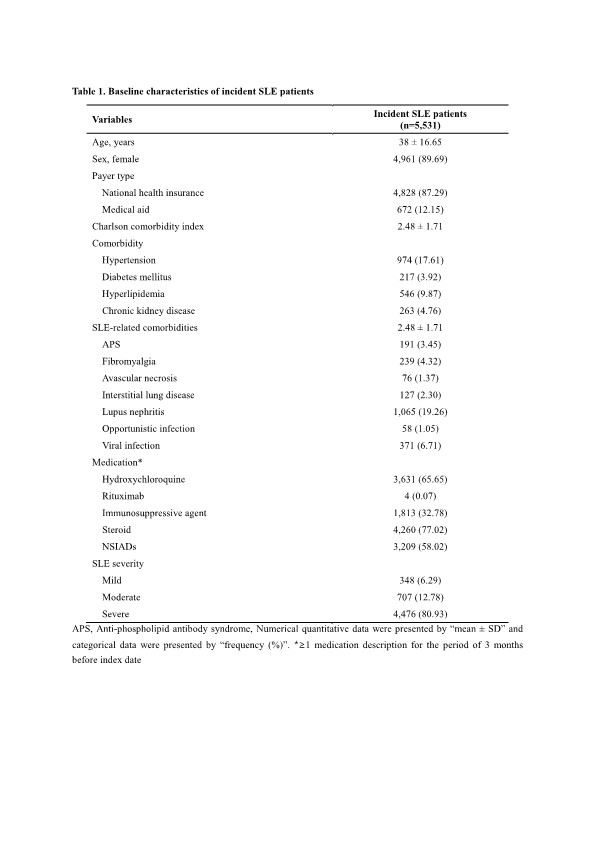
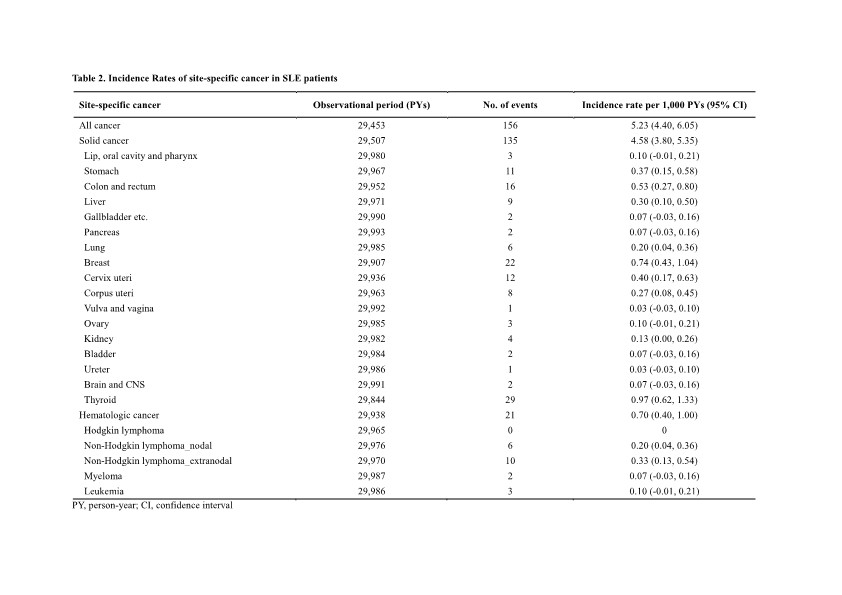
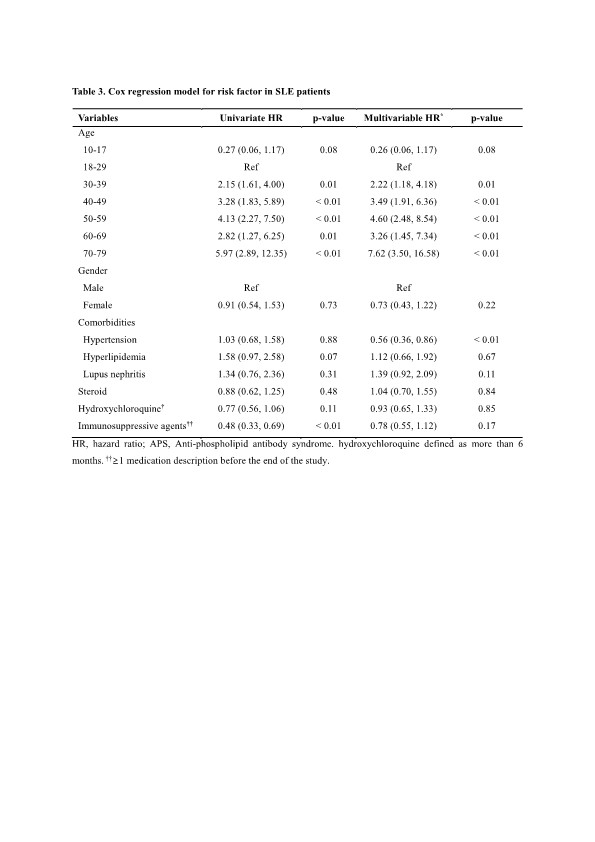
Results: A total of 5,531 patients with newly diagnosed SLE were included, with a mean age of 38.0 ± 16.6 years, and 89.7% of them were female. Table 1 shows the baseline characteristics of the study population. During a follow-up period of 29,453 PYs, 156 SLE patients developed cancer. The IRs per 1,000 PYs for all cancers, solid cancers, and hematologic cancers were 5.23 (95% CI 4.40-6.05), 4.58 (95% CI 3.80-5.35), and 0.70 (95% CI 0.40-1.00), respectively. Based on SEER stage, a higher proportion of SLE patients were diagnosed with solid cancers at localized (64 events) and regional (43 events) stages, rather than distal stage (16 events).Site-specific cancers predominantly included thyroid (0.97, 95% CI 0.62-1.33) and breast cancer (0.74, 95% CI 0.43-1.04), followed by colon and rectal (0.53, 95% CI 0.27-0.80), cervix uteri (0.40, 95% CI 0.17-0.63), and stomach cancer (0.37, 95% CI 0.15-0.58) (Table 2). In the multivariable analysis (Table 3), the risk factors associated with cancer development in incident SLE patients were age above 30 years (adjusted hazard ratio [aHR] 2.22, 95% CI 1.18-4.18), whereas hypertension (aHR 0.56, 95% CI 0.35-0.89) was associated with a lower risk of cancer. Medication, such as hydroxychloroquine and immunosuppressive agents, did not correlate with the risk of cancer.
Conclusion: This study provides insights into the cancer incidence characteristics in Korean patients with newly diagnosed SLE over a long follow-up period. The distribution of cancer incidence was predominantly in the early stages, with thyroid and breast cancers being commonly diagnosed. The risk of cancer increased with older age in SLE patients, while there was no clear association between the use of immunosuppressive agents and cancer.
To cite this abstract in AMA style:
Han J, Jeon Y, Kang G, Jung S, Jang E, Cho S, Sung Y. Cancer Incidence and Risk Factors in Patients with Newly Diagnosed Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/cancer-incidence-and-risk-factors-in-patients-with-newly-diagnosed-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cancer-incidence-and-risk-factors-in-patients-with-newly-diagnosed-systemic-lupus-erythematosus/