Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Ultrasound (US) is superior to clinical examination and can be used for more accurate assessment of joint inflammation in rheumatoid arthritis (RA). However, it is currently unknown if thermography (a safe, low cost and non-invasive imaging modality with high feasibility for use) may be similarly useful. The aim of this study is to evaluate if thermal imaging may help detect joint inflammation, using ultrasound imaging to indicate the status of joint inflammation at clinically quiescent (non-swollen and non-tender) metacarpophalangeal joints (MCPJs).
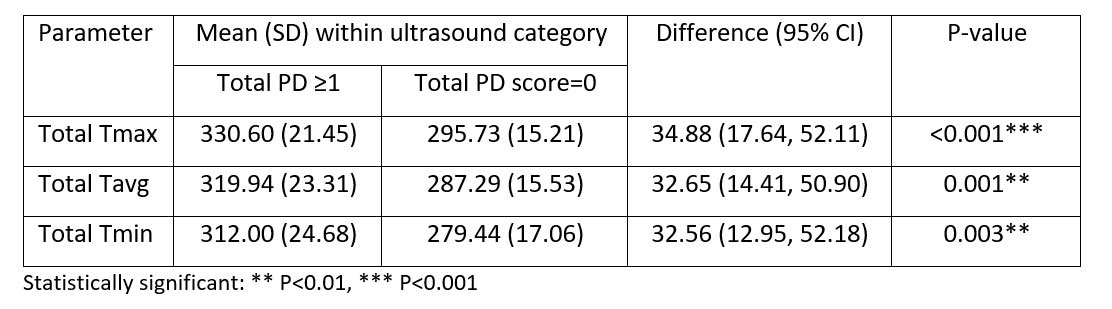
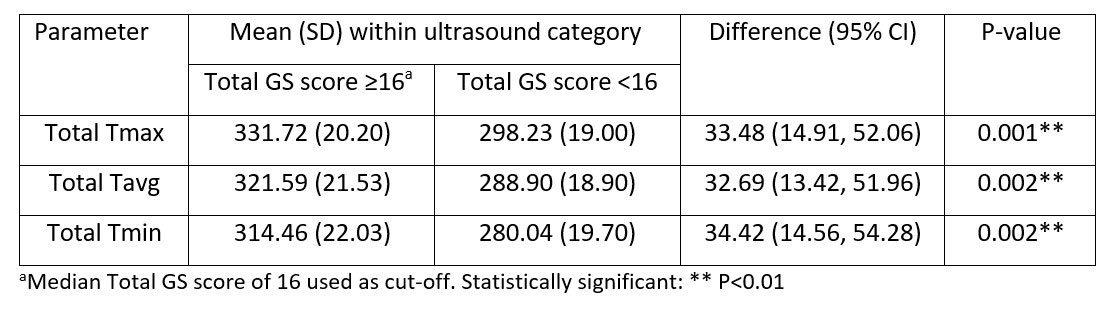
Methods: Thermography and ultrasonography were performed during the same study visit at the bilateral 1st to 5th MCPJs among RA patients who fulfilled the 2010 RA classification criteria and who did not exhibit any joint swelling and tenderness at the bilateral MCPJs. For thermal imaging, the maximum (Tmax), average (Tavg) and minimum (Tmin) temperatures were recorded in °C at the dorsal aspects of each MCPJ. For US, power Doppler (PD) and grey-scale (GS) joint inflammation were graded semi-quantitatively using a 0-3 severity scale at the dorsal joint recesses of the MCPJs. The results for Tmax, Tavg, Tmin, PD score and GS score at the 10 MCPJs were summed up to obtain the respective Total Tmax, Total Tavg, Total Tmin, Total PD score and Total GS score per patient. The Total Tmax, Total Tavg and Total Tmin were then compared (a) between patients who were PD positive (Total PD ≥1) versus those who were PD negative (Total PD score=0) and (b) between patients with Total GS score ≥16 (median Total GS score) versus those patients with Total GS score < 16. The comparative analysis were performed using the Independent Samples T Test.
Results: In this cross-sectional study, 200 non-swollen and non-tender MCPJs were examined among 20 RA patients. The patients’ baseline characteristics are as follows: mean (SD) age, 55.2 (12.4) years, majority were female (17/20, 85%), majority were Chinese (15/20, 75%), mean (SD) disease duration of 7.04 (5.69) months, mean (SD) DAS28 of 3.29 (0.78). Comparing patients who were PD positive (Total PD score ≥1) versus those who were PD negative (Total PD score=0), the differences in mean values (95% CI) for thermographic parameters including Total Tmax, Total Tavg and Total Tmin (Table 1) were 34.88 (17.64, 52.11), 32.65 (14.41, 50.90) and 32.56 (12.95, 52.18), respectively (P-values were all < 0.01). Comparing patients with Total GS score ≥16 (median) versus those with Total GS score < 16, the differences in mean values (95% CI) for thermographic parameters including Total Tmax, Total Tavg and Total Tmin (Table 2) were 33.48 (14.91, 52.06), 32.69 (13.42, 51.96) and 34.42 (14.56, 54.28), respectively (P-values were all < 0.01).
Conclusion: In RA patients with non-swollen and non-tender MCPJs, temperature readings at the MCPJs were significantly higher among patients with positive PD joint inflammation and among those with a greater degree of GS joint inflammation. The role of thermal imaging in clarifying joint inflammation in clinically quiescent MCPJs in RA, as well as other peripheral joint sites, warrants further investigation.
To cite this abstract in AMA style:
Tan Y. Can Thermal Imaging Help Clarify Joint Inflammation at Clinically Quiescent Metacarpophalangeal Joints in Patients with Rheumatoid Arthritis? [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/can-thermal-imaging-help-clarify-joint-inflammation-at-clinically-quiescent-metacarpophalangeal-joints-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/can-thermal-imaging-help-clarify-joint-inflammation-at-clinically-quiescent-metacarpophalangeal-joints-in-patients-with-rheumatoid-arthritis/