Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: The underlying histopathological basis for bone marrow lesions (BML) on magnetic resonance imaging (MRI) in osteoarthritis (OA) is unclear, but may be associated with pain and disease progression. BMLs are visible on fat-suppressed T2 and proton density weighted images by MRI, but not by radiography. It has been proposed that BML reflect hypermetabolic areas characterized by bone remodelling. We aimed to test this hypothesis by combining sequential in vivo micro-MRI with assessment of bone remodelling using a novel dynamic bone labelling methodology employing elemental strontium detection by electron probe microanalysis (EPMA).
Methods: Post-traumatic osteoarthritis (PTOA) was surgically induced in 9 rats, with an additional 3 rats included as sham-operated controls. In vivo micro-MRI images were obtained sequentially at baseline, 4, 8 and 12 weeks after surgery, utilizing 9.4 Tesla T2 and proton density weighted MRI to detect BML. Elemental strontium (sub-therapeutic tracer dosage) was administered daily commencing one day post-surgically until euthanasia at 12 weeks, when strontium incorporation in mineralizing tissues was assessed using EPMA.
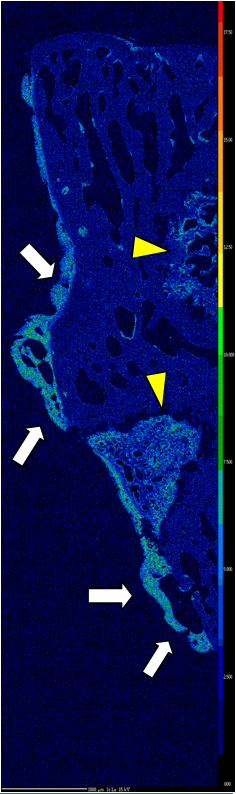
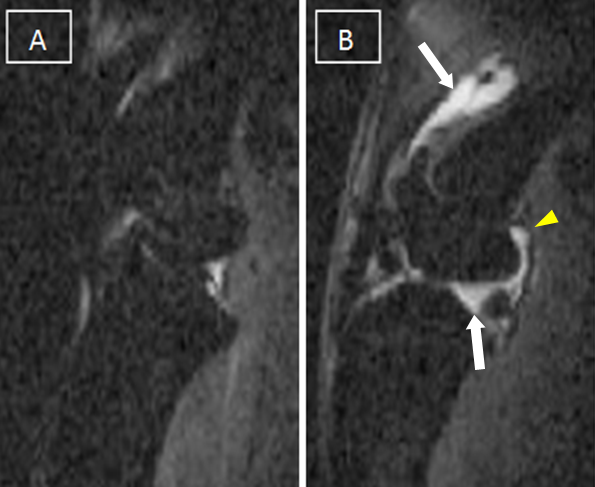
Results: EPMA maps at all time-points demonstrated scant strontium deposition on trabecular surfaces and epiphyseal growth plates, but was most prominently incorporated at sites of developing osteophytes – indicating intensive bone turnover and new bone formation (Fig 1). Joint effusion, synovitis and occasional subchondral cysts were readily visible at 4 weeks under MRI (Fig 2), however, only tiny areas of potential BML-like signal (ill-defined increased T2 signal) were detected in this animal model starting at 4 weeks. Those foci were not located at the sites of strontium incorporation, but were seen at the margins of sub-articular cysts that developed between 4-8 weeks.
Fig 1: EPMA map of untreated rat shows hypermetabolic bone remodelling at joint margins leading to the formation of osteophytes (arrows). Growth plates are depicted with arrow heads.
Fig 2: T2-weighted/fat suppressed MRI at: A) baseline B) 8 weeks exhibiting joint effusion (arrows) and synovitis (arrow head).
Conclusion: In this animal model of PTOA, joint degeneration was associated with florid synovitis, joint effusion, minimal subchondral cyst formation, OA-associated loose body appearance and massive osteophyte formation. In humans, such dramatic arthropathy would generally be accompanied by extensive BML. Although all of the other features of severe OA were present in these animals and hypermetabolism was demonstrated at the joint margins, we detected virtually no BML at 9.4T MRI.
Disclosure:
A. Panahifar,
None;
J. Jaremko,
None;
R. G. Lambert,
None;
W. P. Maksymowych,
None;
M. R. Doschak,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-marrow-lesions-on-magnetic-resonance-imaging-are-not-associated-with-regions-of-hypermetabolism-in-an-animal-model-of-osteoarthritis/