Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Glucocorticoids (GC) are an important mode of therapy in ANCA associated vasculitis (AAV), and osteoporosis (OP) and fractures are potential adverse effects seen. The revised 2017 Glucocorticoid-induced osteoporosis guidelines by the American College of Rheumatology (ACR) categorizes patients into low, moderate and high fracture risk groups and provides recommendations. Our aim was to analyze the implementation of the guideline in AAV patients. This was a quality improvement (QI) initiative to identify potential targets for improving practice.
Methods: Patients with vasculitis (AAV) were identified in 2 academic centers by generating an electronic medical record query during the period of 2012-2019. Patients with inadequate information at baseline and follow up, steroid use of < 3 months and steroid naive patients were excluded. 56 patients were included in the study. Demographics, OP risk factors, duration and dose of GC, bone mineral density (BMD) results were collected. Guideline adherence was assessed by analyzing the following: obtaining baseline DXA, testing of vitamin D levels, calcium and vitamin D supplementation and initiation of OP therapy. Fisher’s exact test was used to determine if proportional differences existed in tests ordered between patients ≥ and < 40 yrs
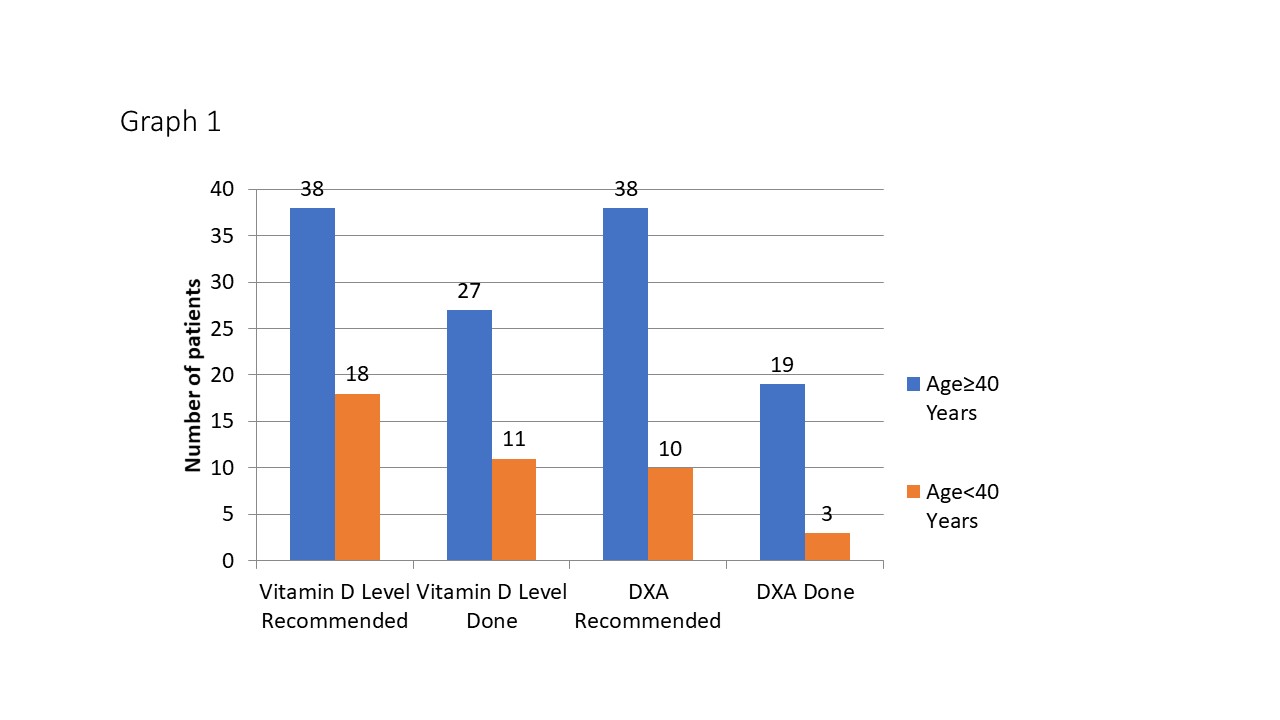
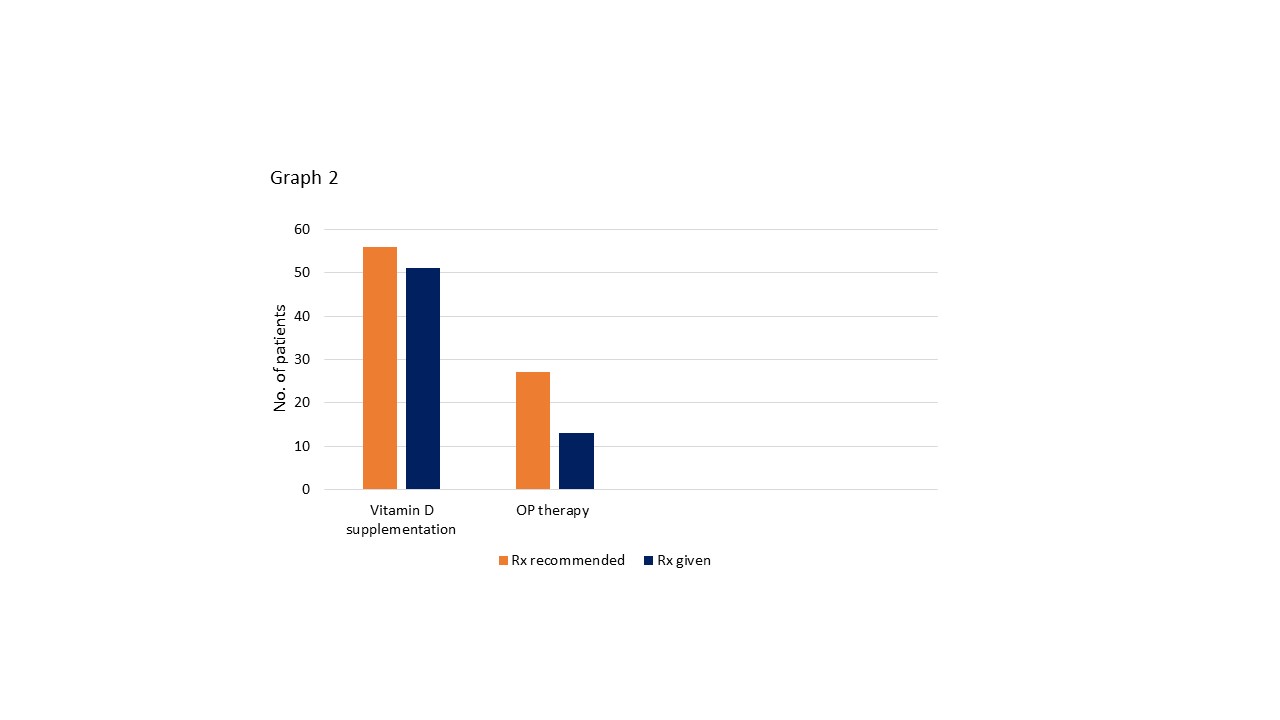
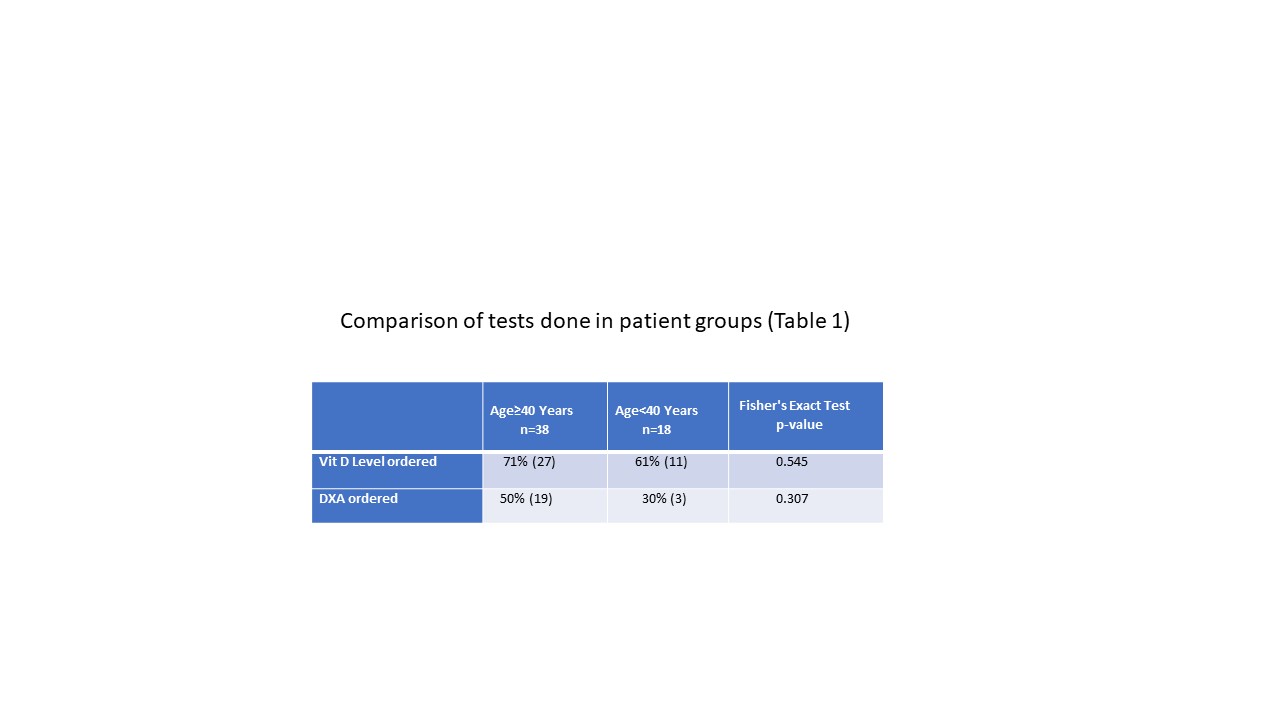
Results: The mean age of the patients was 52.16 yrs (range 16 – 84 yrs) with 67.8 % (n=38) being females. Majority (n= 31, 59.6%) were on steroids for > 1 yr; with minimum duration of 3 months and minimum initial dose of 5 mg. Six (11.5%) had prior OP fracture. Though DXA is recommended in all patients ≥ 40 yrs, only 50% (n=19) had BMD tested (graph 1). 50 % (n=10) had OP and 64.7% were treated with bisphosphonates, 20% by denosumab and 10% by teriparatide. No prior OP fracture was seen in patients < 40 yrs. 56% (n= 10) met criteria based on OP risk factors for BMD testing at baseline and only 30% (n=3) were tested (graph 1). 43.7% also met BMD screening criteria based on cumulative steroid dose, however none of them underwent testing. There was no significant difference in ordering of DXA tests between the 2 age groups (p=0.307, table 1). 92.3% were advised calcium and vitamin D supplementation, however only 67.8 % had the levels checked (see graph 1) and there was no statistically significant difference in ordering of Vitamin D levels between the age groups (Table1). 69.2% of patients were in high and moderate fracture risk group that met criteria for OP therapy and only 33.3% received pharmacologic therapy (see graph 2). Patients < 40 yrs on continued GC dose of > 7.5mg/day for > 6 months have moderate fracture risk based on BMD (z score < 3, rapid bone loss >10%). Due to inadequate BMD testing in patients < 40 yrs, risk stratification for pharmacologic therapy could not be done.
Conclusion: GIOP is a potentially reversible condition. In the study however, adherence to the guideline was inadequate in regards to ordering baseline DXA, checking vitamin D levels and starting OP therapy in high and moderate risk patients, especially in patients < 40 yrs. Hence this project identifies a potential QI initiative that can be implemented to improve the above practice methods in patients treated with long term steroids for many rheumatological conditions not just limited to vasculitis.
To cite this abstract in AMA style:
Ragesh Panikkath D, Lee S, Downey C. Bone Health in ANCA – Associated Vasculitis Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/bone-health-in-anca-associated-vasculitis-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-health-in-anca-associated-vasculitis-patients/