Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patient research partners (PRPs) participate in research teams and provide unique and valuable input. Their integration as equal partners is recommended (1). However, PRP involvement still faces significant challenges that need to be addressed (2). This study aimed to assess PRPs’ roles, identify barriers to their involvement, and propose strategies to improve involvement.
Methods: A systematic literature review was conducted in PubMed/Medline, focusing on studies reporting PRP involvement in rheumatology published between 2017 and January 2023. Keywords such as “patient research partner,” “patient expert,” “patient and public involvement (PPI)”, and relevant acronyms (PRP, PPI) were used. Data collection encompassed quantitative and qualitative data on PRP definition, roles, added value, and barriers and facilitators to their involvement. The analysis included descriptive statistics for quantitative data (frequencies, n%) and inductive thematic analysis for qualitative data.
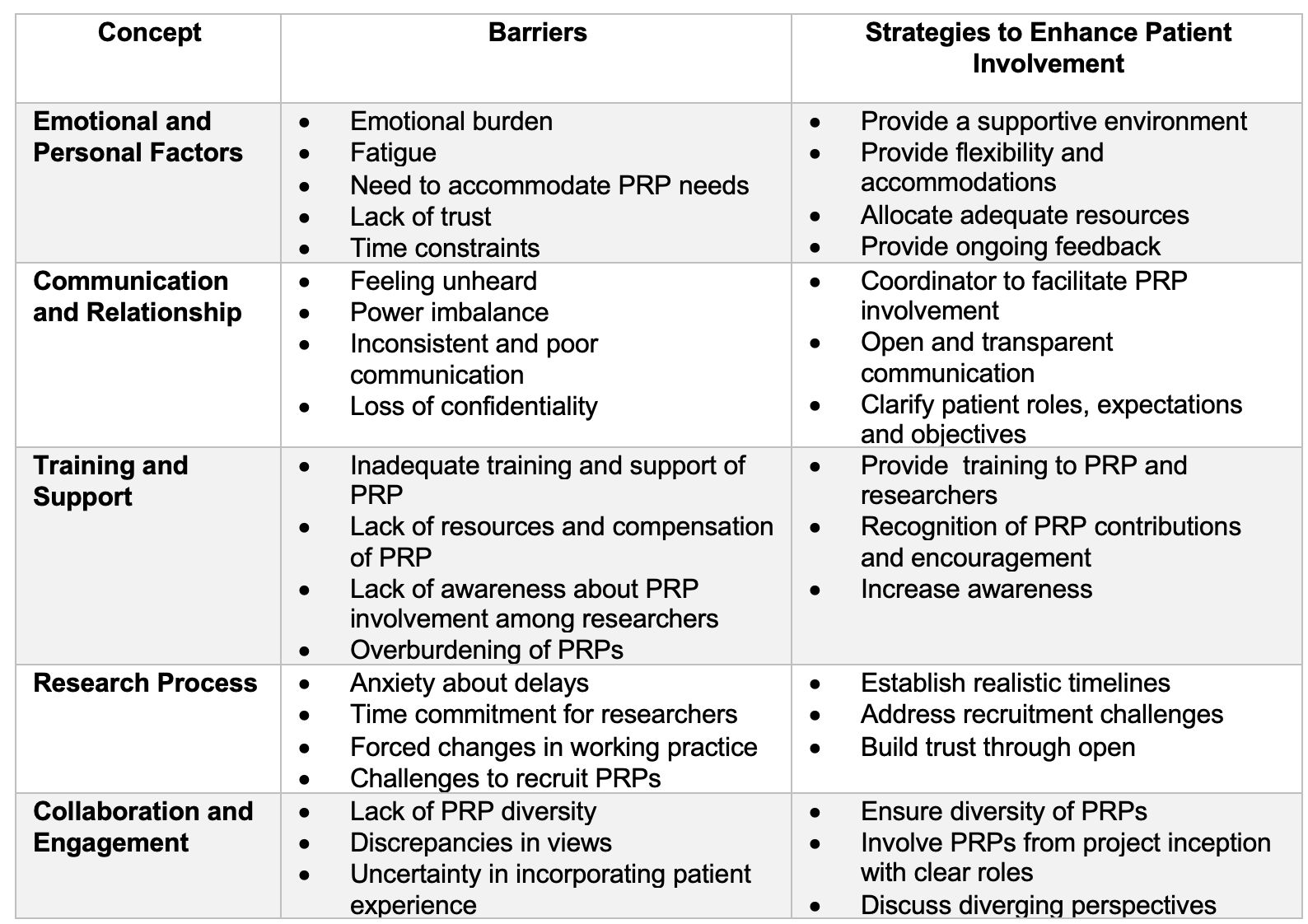
Results: A total of 1481 studies were identified, 108 full-text articles were assessed for eligibility, and 53 were included. Among these, 69% were qualitative studies, reviews, opinion papers, or reports, with 62% published in rheumatology journals. Geographically, 50% of the studies were from Europe, and 31% from North America. 60% of articles reported a definition of PRPs identifying terms such as “equal partnership”, “active engagement”, and “collaboration with researchers”. When PRP involvement was reported, the number of PRPs per project ranged 1 to 4 in 51% of the articles and more than 5 PRPs in 25% of the articles. Various roles of PRPs were described ranging from research partners to patient advocates, advisors, and patient reviewers. PRPs were reported to be involved in all phases of research in 30% of papers, from the conception, conduct to the implementation of outcomes. Barriers to PRP involvement (Table 1) included emotional and personal factors, communication and relationship challenges, inadequate training and support, difficulties following the research process and pace, as well as collaboration and engagement issues. Effective strategies to enhance PRP involvement (Table 1) included early involvement, a supportive environment, effective communication and trust, and providing support and training for PRPs and researchers.
Conclusion: This systematic literature review identified barriers and proposes solutions to enhance PRP involvement in rheumatology research. Addressing these barriers and implementing effective strategies is crucial for meaningful PRP involvement. Further efforts are needed to promote and facilitate patient engagement in research to ensure its relevance and impact.
References
1) de Wit MP, et al. European League Against Rheumatism recommendations for the inclusion of patient representatives in scientific projects. Ann Rheum Dis. 2011.
2) Studenic P et al. Unmet need for patient involvement in rheumatology registries and observational studies: a mixed methods study. RMD open. 2019.
To cite this abstract in AMA style:
Aouad K, de Wit M, Elhai M, Benavent D, Bertheussen H, Primdahl J, Zabalan C, Studenic P, Gossec L. Barriers and Strategies to Enhance Patient Research Partner Involvement in Rheumatology Research: A Systematic Literature Review [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/barriers-and-strategies-to-enhance-patient-research-partner-involvement-in-rheumatology-research-a-systematic-literature-review/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/barriers-and-strategies-to-enhance-patient-research-partner-involvement-in-rheumatology-research-a-systematic-literature-review/