Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose:
Little is known of the characteristics of psoriatic spondyloarthritis (PsSpA). A study was conducted to determine the: (i) prevalence of PsSpA in a psoriatic arthritis (PsA) cohort; (ii) clinical and radiographic characteristics of PsSpA.
Methods:
A prospective single-centre cross-sectional observational study was conducted, recruiting consecutive patients: 201 PsA (CASPAR+) and 201 ankylosing spondylitis (AS; modified New York, mNY+). Participants were examined clinically, completed patient reported outcome measures, and their axial radiographs (cervical, lumbar, pelvis) were scored. Multivariate Poisson regression analyses are presented.
Results:
The 402 enrolled cases were reclassified on the basis of radiographic axial disease and psoriasis: 118 PsSpA, 127 peripheral-only PsA (pPsA), and 157 AS cases (40, 7, and 89% were HLA-B27+, respectively). The prevalence of PsSpA in this SpA cohort was 118/245 (48%).
CASPAR criteria were fulfilled by 49/201 (24%) AS cases, and mNY criteria by 48/201 (24%) PsA cases.
Symptomatically-silent PsSpA (radiographic but no recall of symptoms) was present in 30/118 (25%) of PsSpA cases. Of 118 PsSpA cases: 45/118 (38.14%) had sacroiliitis and spondylitis; 34/118 (28.81%) had sacroiliitis alone; and 39/118 (33%) had spondylitis without sacroiliitis.
Younger age at arthritis symptom onset (p=0.01) and psoriatic nail crumbling (adjusted incidence risk ratio, aIRR 2.86; 95%CI 1.67, 5.00; p<0.001) predicted the occurrence of PsSpA.
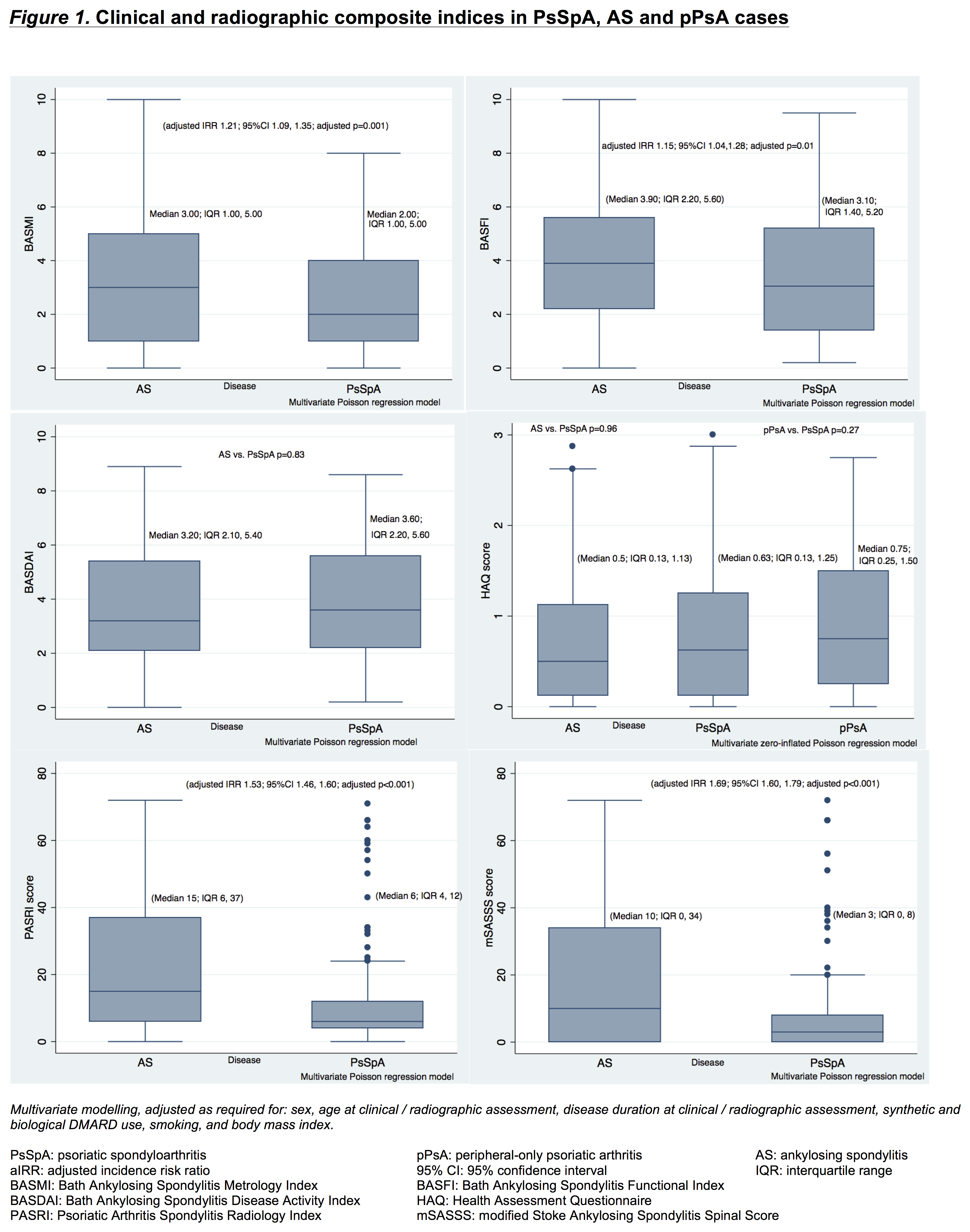
PsSpA cases had similarly high disease activity (ASDAS, BASDAI) to that seen in the AS cases (Figure 1). Disability (HAQ) was no different across the three groups. Function (BASFI, aIRR 1.15; 95%CI 1.05, 1.28; p=0.01) and axial metrology (BASMI, aIRR 1.21; 95%CI 1.09, 1.35; p=0.001) were poorer in AS than PsSpA cases.
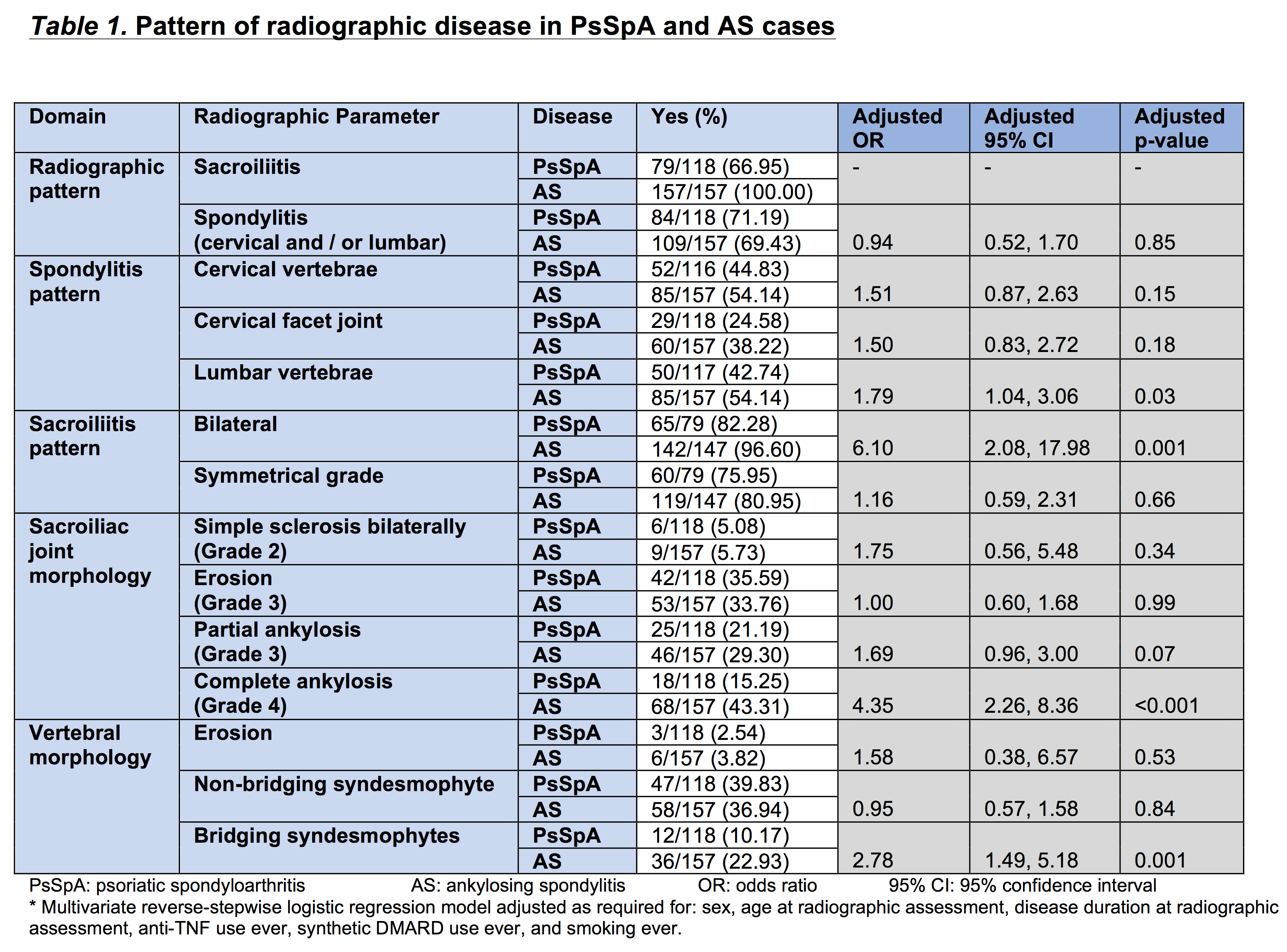
Both AS and PsSpA cases predominantly have bilateral symmetrical-grade sacroiliitis, and both cervical vertebral and facet spondylitis. Complete SIJ ankylosis (aOR 4.35; 95%CI 2.26, 8.36; p<0.001) and bridging syndesmophytes (aOR 2.78; 95%CI 1.49, 5.18; p<0.001) were more likely in AS than PsSpA cases. Radiographic severity was higher in AS compared with PsSpA cases (mSASSS score, aIRR 1.69; 95%CI 1.60, 1.79; p<0.001; PASRI score, aIRR 1.53; 95%CI 1.46, 1.60; p<0.001).
Conclusion:
PsSpA was more prevalent than expected. Symptomatically-silent PsSpA, and spondylitis without sacroiliitis are important considerations when classifying PsSpA. PsSpA has as severe a clinical impact as AS, but is radiographically less severe. Bridging syndesmophytes and complete SIJ fusion appear to best radiographically differentiate PsSpA from AS.
To cite this abstract in AMA style:
Jadon DR, Sengupta R, Nightingale AL, Lindsay M, Korendowych E, Robinson G, Jobling A, Shaddick G, Barton A, McHugh NJ. Axial Disease in Psoriatic Arthritis: A Clinical and Radiographic Comparison with Ankylosing Spondylitis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/axial-disease-in-psoriatic-arthritis-a-clinical-and-radiographic-comparison-with-ankylosing-spondylitis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/axial-disease-in-psoriatic-arthritis-a-clinical-and-radiographic-comparison-with-ankylosing-spondylitis/