Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Average diagnostic delay for axial spondyloarthritis (axSpA) is 7 to 10 years. Lack of timely referral of inflammatory back pain (IBP) patients by non-rheumatology physicians (non-rheums) is an important contributor. We systematically surveyed non-rheums in the US to assess their knowledge, awareness, and attitudes towards axSpA. The objective is to identify barriers for referral and opportunities for intervention.
Methods: An online survey questionnaire was developed and refined using input from previous smaller regional study, methodologists and pilot testing. Survey included demographic information, practice patterns, questions about the knowledge and approach towards IBP and axSpA. Survey was distributed to non-rheums taking care of chronic back pain (CBP) patients namely Family/Internal Medicine, Spine Surgery/Orthopedics, Pain Medicine, and Physical Medicine/Physiatry/Rehabilitation across the US using third party vendor. Survey was also sent to rheumatologists (rheums) who served as comparator group. Descriptive statistics was used, and Pearson’s chi-squared test was used to compare categorical variables
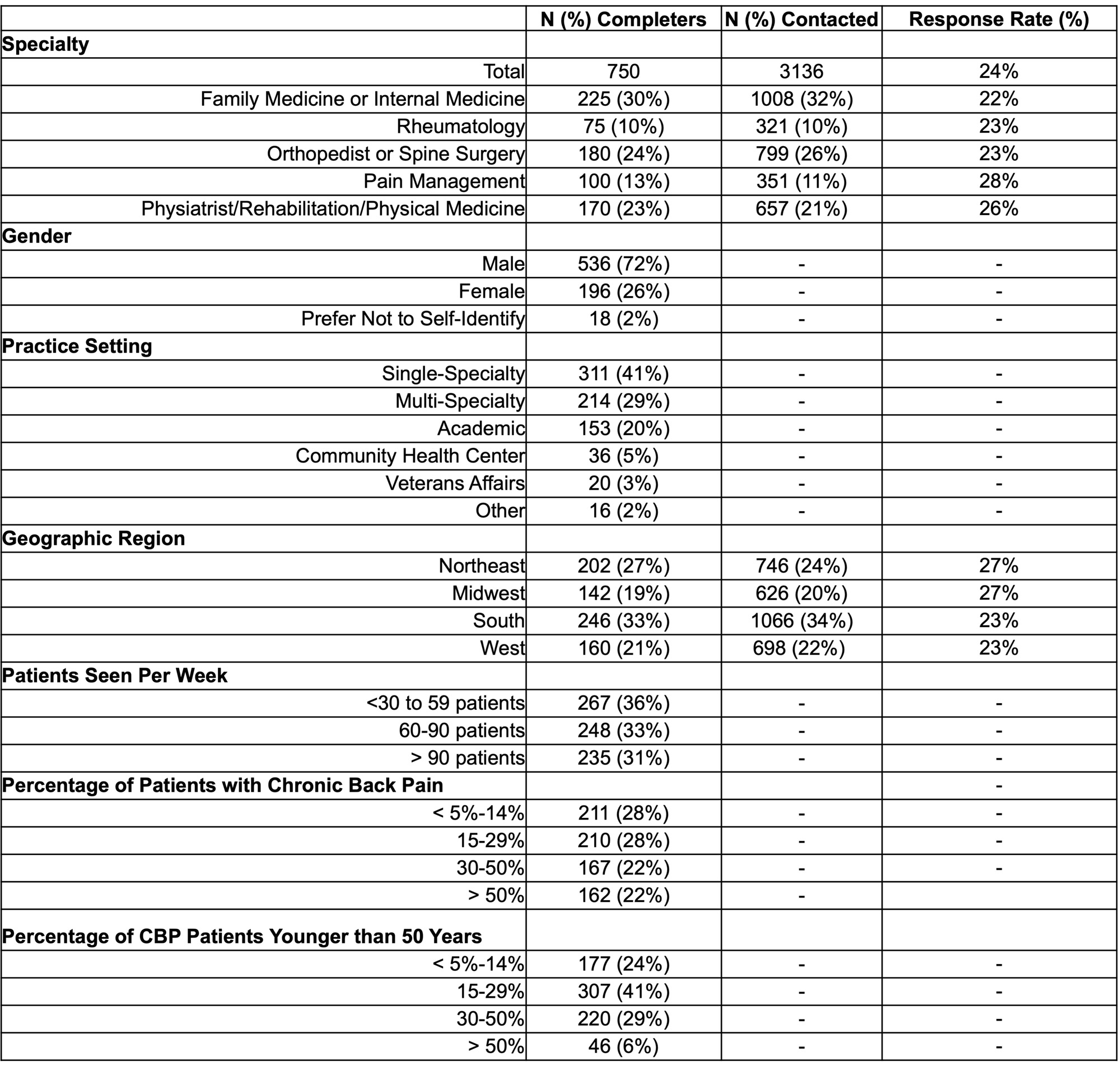
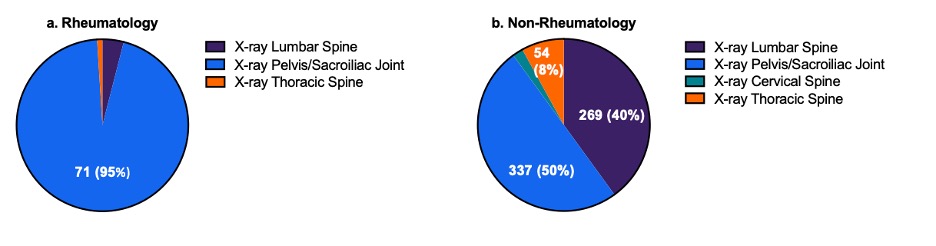
Results: Of 3136 physicians who received the survey, 750 completed it (response rate 24%). Table 1 shows baseline information of respondents. Physicians were in various practice settings (42 % single specialty, 29% multi-specialty, 20% academics) and varying post-training experience (40% < 5-15 years, 40% 15-30 years, and 10% > 30years). CBP was commonly reported; 72% physicians reported CBP in >15% of their patients and 44% in >30% patients. While majority (75%) of non-rheums were familiar with IBP and 87% recognized >4 of 8 IBP items, only 40% routinely assess for IBP in clinical practice. Non-rheums screen CBP patients for inflammatory arthritis, IBD and family history of SpA for only 50% of the times and even less often for heel enthesitis, uveitis and psoriasis (see Table 2) as compared to rheums. Non-rheums also order the CRP and HLA-B27 significantly less often in CBP patients compared to rheums. Non-rheums usually/always order ANA and RF in 47% and 52% IBP patients; rheums order these in 27% and 35% patients respectively. Only 50% of non-rheums correctly answered x-ray SI/pelvis as initial imaging test of choice in suspected axSpA. MRI pelvis was selected as next imaging test by only 37% non-rheums. Non-familiarity with term axSpA and nr-axSpA was reported by 11% and 35% non-rheums respectively. Non-rheums less often (p value < 0.0001) consider axSpA/AS as a possible diagnosis in CBP patients; 20% never or rarely do it and 49% do it sometimes. Formal referral guidelines for axSpA patients were felt important or very important by 81% non-rheums and 97% rheums.
Conclusion: In this large nationwide survey study involving different specialists caring for CBP patients, we found that there is lack of knowledge and awareness about nomenclature, lab testing, and proper imaging in suspected axSpA patients. Unnecessary lab tests are commonly ordered in CBP patients by non-rheumatologists and also to an extent by rheumatologists. Formal referral guidelines and improved education may help in reducing the diagnostic delay of axSpA.
To cite this abstract in AMA style:
Odell W, Alexander S, Page N, Maheshwari N, Danve A. Awareness and Attitudes Regarding Axial Spondyloarthritis Among Non-Rheumatology Physicians in the United States [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/awareness-and-attitudes-regarding-axial-spondyloarthritis-among-non-rheumatology-physicians-in-the-united-states/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/awareness-and-attitudes-regarding-axial-spondyloarthritis-among-non-rheumatology-physicians-in-the-united-states/