Session Information
Date: Wednesday, November 15, 2023
Title: Abstracts: Miscellaneous Rheumatic & Inflammatory Diseases III
Session Type: Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: The term interstitial pneumonia with autoimmune features (IPAF) describes patients with interstitial lung disease (ILD) and features of autoimmunity, that do not fulfill classification criteria for any of the defined rheumatic diseases (RD) or for other ILD subtypes. While cases of progressive ILD with clear autoimmune etiology such as those associated with RDs are usually treated with immunosuppression, IPAF, due to its heterogeneity and unclear pathophysiology, presents substantial difficulty in management. Our overarching hypothesis is that there are unique autoantibody profiles that can be identified in autoimmune forms of ILD reflecting the underlying inflammation-mediated damage. Understanding these signatures will allow us to identify an autoimmune endotype within poorly characterized ILD types such as IPAF with potential therapeutic implications.
Methods: We conducted a cross-sectional analysis of patients with RD-ILD (n=32) and idiopathic pulmonary fibrosis (IPF) (n=69) to evaluate autoantibodies correlating to autoimmune driven ILD (defined as RD-ILD). Autoantibody profiles were determined using a fluorescence-based multiplex assay for the detection of 124 IgM and IgG autoantibodies that detect autoantigens important in rheumatic diseases and ILD in the prior literature. T-test with False Discovery Rate (a=0.05) was performed to investigate significant mean differences between RD-ILD and IPF to identify autoantibodies characteristic of RD-ILD versus IPF, controlling for minimum detection level with censored regression methods. LASSO logistic regression was performed to identify autoantibodies predictive of RD-ILD subtype versus IPF subtype. A longitudinal cohort study was performed to evaluate association of autoantibodies with lung disease progression (defined as relative forced vital capacity (FVC) decline of 10% or more, death, or lung transplant). Cox logistic regression was utilized to assess the association of autoantibodies with time to progression within each ILD subtype.
Results: Seven autoantibodies were selected by both FDR and LASSO methods, with additional autoantibodies selected by one of the other two methods. Ro-52 SSA IgG, U1snRNP IgG, nucleosome antigen IgM, SM-D1 IgM, proteoglycan IgM, and histone H1 IgG autoantibodies showed highest relevance score for association with RD-ILD versus IPF subtype (Figure 1).
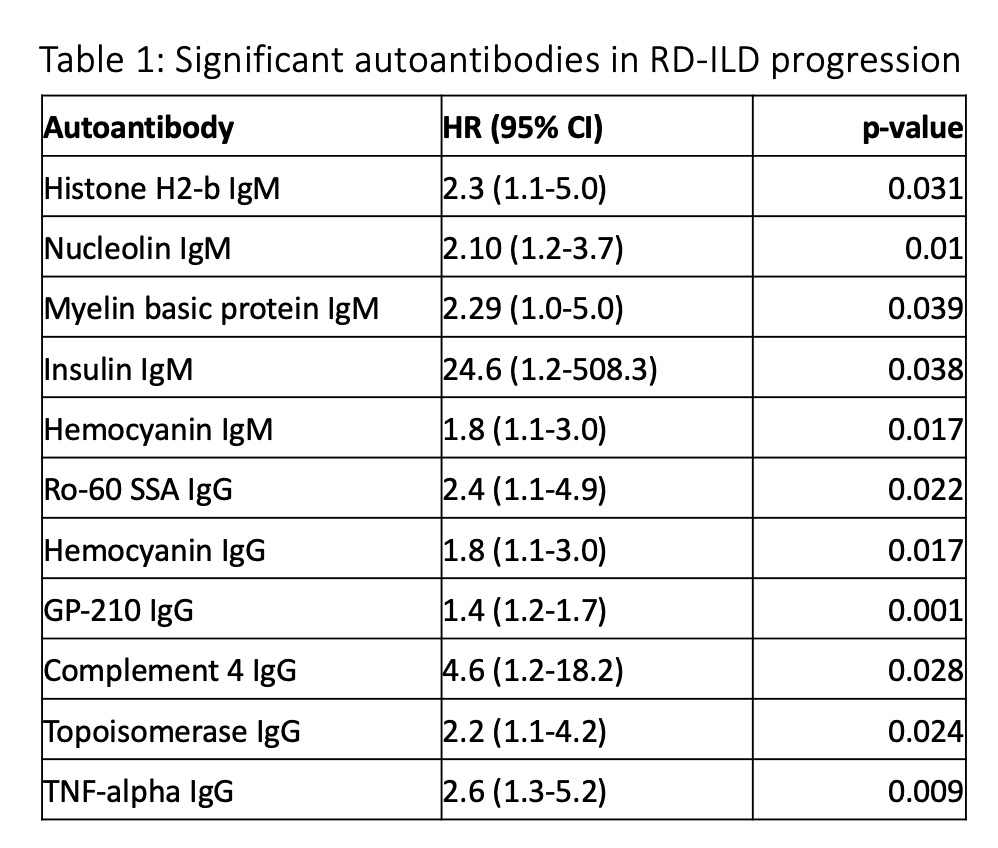
In RD-ILD, 11 autoantibodies were significantly associated with faster progression, while in IPF, six autoantibodies were significantly associated with the outcome.
Conclusion: Several autoantibodies appear to be associated with RD-ILD more than IPF. Greater autoantibody level elevation in RD-ILD than in IPF emphasizes the lack of autoimmunity in the IPF patients. Different autoantibodies were associated with progression in RD-ILD and IPF, suggesting different mechanisms of damage. Autoantibodies predicting faster progression in IPF patients emphasized potentially undiagnosed autoimmune ILDs among IPF patients and the need for broad testing in a variety of ILDs. Knowledge of autoantibody profiles associated with autoimmune lung disease and progression in various ILD subtypes has implications for management decisions in ILD.
To cite this abstract in AMA style:
Joerns E, Newton C, Kolenikov S, Sparks J, Karp D. Autoantibody Profile of Autoimmune Driven Interstitial Lung Disease as Compared to Idiopathic Pulmonary Fibrosis and Association of Autoantibodies with Survival [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/autoantibody-profile-of-autoimmune-driven-interstitial-lung-disease-as-compared-to-idiopathic-pulmonary-fibrosis-and-association-of-autoantibodies-with-survival/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibody-profile-of-autoimmune-driven-interstitial-lung-disease-as-compared-to-idiopathic-pulmonary-fibrosis-and-association-of-autoantibodies-with-survival/