Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Interstitial lung disease (ILD) significantly contributes to morbidity and mortality in adult polymyositis (PM) and dermatomyositis (DM). Myositis associated autoantibodies (MAA) are associated with unique clinical phenotypes and patient outcomes. In particular, the anti-tRNA synthetase autoantibodies (anti-synAbs) are associated with high rates of ILD. Our aim was to determine predictors of survival in myositis associated ILD (MA-ILD) and to evaluate differences related to autoantibody (autoAb) subsets.
Methods: PM and DM subjects with ILD or with the antisynthetase (anti-syn) syndrome with ILD were consecutively identified from the University of Pittsburgh (UPITT) CTD registry which encompasses more than three decades of prospective data linked to a sample repository collected on outpatients and inpatients with various autoimmune diseases. PM and DM patients met probable or definite Bohan and Peter criteria and the anti-syn patients possessed one of the 8 known anti-syn autoAbs (i.e. anti-Jo-1, PL-7, PL-12, EJ, OJ, KS, Zo and Tyr). ILD was radiographically defined by characteristic xray or high-resolution computerized tomography findings. Death or transplant was determined from the registry or electronic medical record. Kaplan Meier and log rank tests were used to determine survival rates and differences between autoAb groups. Cox proportional hazards model was used to determine survival differences after controlling for co-variates including age at diagnosis, gender, ethnicity and baseline FVC%.
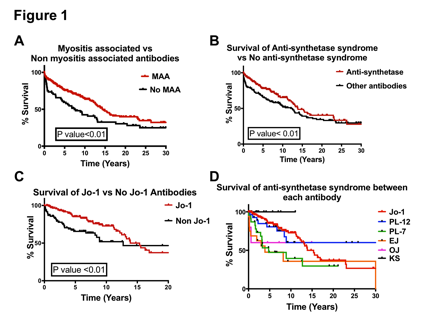
Results: 369 patients met criteria for MA-ILD and 306 (83%) had positive autoAbs. Overall, 63% (231/369) had MAAs and 54% (198/369) had a positive the anti-syn autoAb. The most common autoAb subset in the entire autoAb (+) cohort was anti-Jo-1(124/306; 41%). The overall 5 and 10 year survival of MA-ILD was 80% at 5 years and 72% at 10 years. Patients with an MAA had better survival compared to MAA (-) subjects (5 and 10 year survival 80% vs. 72%; 72% vs. 58%, p=0.003). Among MAA (+) patients, those with anti-syn autoAbs had better survival compared to those with non-anti-syn autoAbs (5 and 10 years survival 80% vs. 73%; 73% vs. 61%, p=0.004). Among the entire anti-syn autoAb (+) subjects, those with anti-Jo-1 had a better survival than those patients with 1 of the 7 other anti-syn autoAbs (5 and 10 year survival 86% vs. 72%; 77% vs. 65%, p=0.04).
Conclusion: Myositis patients with MAA, particularly anti-syn autoAbs have better survival rates compared to those without autoAbs. Among anti-syn autoAb (+) patientÕs Jo-1 positivity confers a better survival. Myositis-associated autoAbs predict survival and long-term prognosis in myositis.
To cite this abstract in AMA style:
Martinez S, Aggarwal R, Oddis CV. Autoantibodies Predict Long Term Survival in Myositis Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/autoantibodies-predict-long-term-survival-in-myositis-associated-interstitial-lung-disease/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibodies-predict-long-term-survival-in-myositis-associated-interstitial-lung-disease/